We help health care organizations succeed in risk-based arrangements
Request a Demo
Improving Care Delivery, Population Health & Financial Performance
Proprietary Algorithms
ARC uses proprietary algorithms to drive actionable intelligence and initiatives across care management, coordination, provider-focused network incentives and premium enhancement to optimize performance
Financial Success
ARC enables providers and payers to confidently chart a financially viable course to accept more risk-based payments while driving better quality, outcomes and costs
Performance Reporting
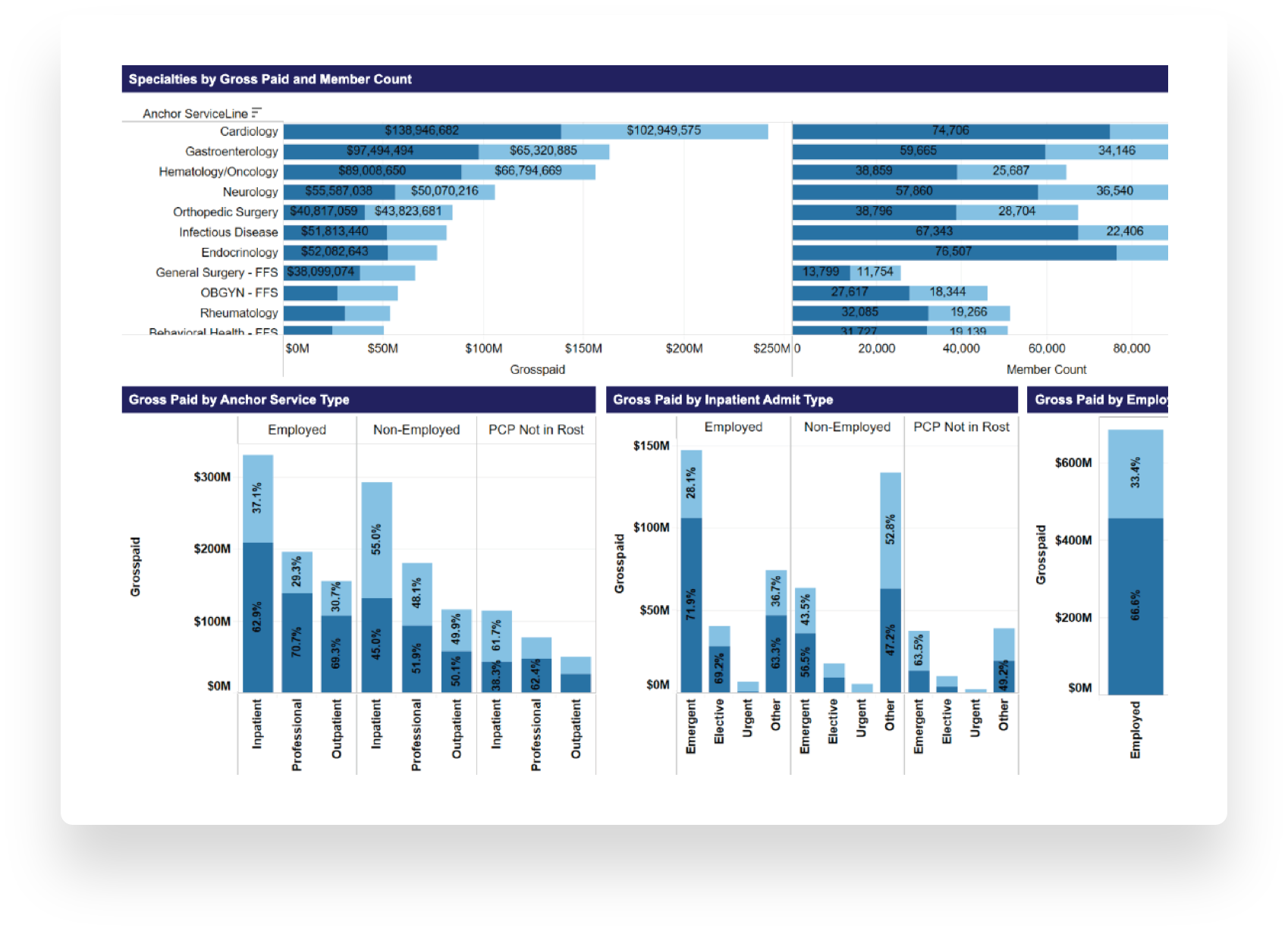
Providers and payers see how they are performing against care delivery and financial plans
The analytics platform delivers precise information and detailed insight from its comprehensive data inputs and analytical power.
-
Aggregate Data
Aggregates data from numerous sources across the continuum of care and populations—claims, pharmaceutical, provider financials, SDOH, biometrics and national, regional and network benchmarks -
Transform Data
Transforms, sorts, slices and analyzes data into actionable insights, such as network gaps, high-risk members or therapy effectiveness based on risk factors such as patient age and comorbidities -
Provide Solutions
Provides root causes and paths for navigating to solutions after flagging specific problems or variations within populations, service lines, clinicians or locations
Develop a roadmap to economic success in value-based contract arrangements
Operationalize value-based agreements by identifying targeted opportunities to implement initiatives to better manage a population
Tailor initiatives that consider and meet local and regional market nuances
Draw on a library of provider use cases to enhance learning for all and gain more buy-in
Forecast the financial impact of population health initiatives and aligned incentive models for providers on risk pool and provider performance
Coordinate care with dashboards for team—physicians, pharmacists, network managers, care coordinators, post-acute/CBOs, finance, leadership
Create internal and leverage external benchmarking methodologies to facilitate change in physician and other provider approaches to care delivery
Access disparate data sources, advancing data interoperability goals
Serving 7 Health Plans and 5 Provider Clients
Data from 2.5 million members
In 6 states and growing
- Identify strategies to manage total cost of care across aggregated or individual contracts, lines of business, contracting entities, risk pods, physician panels, hospitals and other provider types
- Evaluate primary care and specialty care physician performance in order to optimize contracted and referral networks
- Leverage chronicity, social determinants of health (SDOH), biometric, pharmacy and other data for advanced risk stratification, chase lists and population health management
- Increase revenue through membership growth, service expansion, appropriate documentation and – under capitation or global risk arrangements – maximization of non-premium revenues
- Generate plan reporting with drill down into cost and use
- Accelerate provider engagement and improve performance in value-based payment arrangements
- Match financial data to service utilization and trends to provide actionable insights along with performance data for physician practices
- Evaluate primary care and specialty care physician performance in order to optimize contracted and referral networks
- Leverage chronicity, social determinants of health (SDOH), biometric, pharmacy and other data for advanced risk stratification, chase lists and population health management
- Gain transparency to total cost of care and levers to manage it
- Enhance benefits design, improve convenience and beneficiary satisfaction scores through a better understanding of patterns of care
- Gain insights to establish value add direct contracts with high performing providers and Centers of Excellence
- Evaluate primary care and specialty care physician performance in order to optimize contracted and referral networks
- Leverage chronicity, social determinants of health (SDOH), biometric, pharmacy and other data for advanced risk stratification, chase lists and population health management
- Assess efficacy and ROI of drug therapies for specific cohorts in relation to total cost of care
- Identify additional patient segments who may benefit from existing drug therapies
- Facilitate developing value-based payment contracts with payor and provider partners
- Run medical and pharmacy claims, SDOH, biometrics and other cost accounting data to understand historical performance and set realistic forecasts to manage costs
- Enable scenario modeling of population health management levers to arrive at effective contract terms
- Showcase intervention efficacy and quantify their contribution to managing the total cost of care for relevant cohorts
- Identify providers who deliver optimal value for members
- Benchmark within your own provider population to identify best-in-class performance and help raise the effectiveness of underperformers
- Provide performance reporting to provider groups to support total cost of care management initiatives
- Understand key provider partners who are managing high-need member populations
- Uncover opportunities to better manage populations
- Identify high-performing providers within your network to acquire best practices and share with the rest of your providers
- Review historical trends to build a network that meets the current and future needs of members
- Find network leakage and create programs for reducing out-of-network spend
- Develop and evaluate high-performing specialty networks to concentrate referrals
“We are excited to be working with the ARC team to identify additional opportunities for improvement. This will enable us to continue to add greater value to our members, our parent company Travis County Healthcare District and to the greater community.”

Wesley Durkalski
President and Chief Executive Officer for Sendero Health Plans
“Using its years of population health management experience and ARC, Montefiore’s Care Management company found opportunities to reduce single-day admissions, admissions for end stage renal disease, improve in-network referral, and reduce overall cost of specialty care.”

Stephen Rosenthal
President
Care Management Company, a subsidiary of Montefiore Health System
“Within two weeks of using ARC, we identified several large opportunities for improvement. We prioritized the most pressing ones and have begun the process to revise hospital contracts to generate annual savings going forward.”

John Beaman
Chief Business Officer
Adventist Health
ARC is a subsidiary of COPE Health Solutions
ARC is a subsidiary of COPE Health Solutions, formed through a joint venture between COPE Health Solutions, Montefiore Health System, Adventist Health and Dr. Richard Merkin, owner of Heritage Provider Network Inc. Montefiore Health System and Adventist Health have been strategic partners with COPE Health Solutions in developing and using the cloud-native ARC tool.
ARC is available as a software as a service platform, with the option of working with COPE Health Solutions to analyze data, develop insights, understand the financial consequences and plan and execute improvement efforts.
Press Release: ARC Expands Client Portfolio with the Addition of Sendero Health Plans