 On May 1, 2016, the Centers for Medicaid and Medicare Services (CMS) approved a 15-month temporary extension for Texas’ Section 1115 Medicaid Transformation Waiver. This is the first extension and it will serve as an opportunity for the state to preserve the existing Delivery System Reform Incentive Program (DSRIP) as it continues to negotiate a longer-term waiver renewal with CMS. Throughout this extension and renewal process, the state has been releasing information on proposed rule changes for providers with DSRIP projects.
On May 1, 2016, the Centers for Medicaid and Medicare Services (CMS) approved a 15-month temporary extension for Texas’ Section 1115 Medicaid Transformation Waiver. This is the first extension and it will serve as an opportunity for the state to preserve the existing Delivery System Reform Incentive Program (DSRIP) as it continues to negotiate a longer-term waiver renewal with CMS. Throughout this extension and renewal process, the state has been releasing information on proposed rule changes for providers with DSRIP projects.
This temporary extension will last 15 months after the previously planned end of the waiver, from October 1, 2016 to December 31, 2017. In this interim timeframe between the current waiver rules and the proposed revisions, providers are navigating murky waters between carrying out their current project goals and preparing for the upcoming changes. This article will discuss a select few proposed waiver rule changes, how they will impact providers and how providers can prepare for these changes.
For more information on the waiver renewal, please refer to the Texas Health and Human Services Commission (HHSC) website here.
Proposed change: Medicaid and low-income uninsured patient inclusions
Currently, providers are required to track provision of services by payor, to identify percentage of services given to Medicaid or low-income uninsured patients (notice that patients must be both low-income and uninsured to qualify), also known as the MLIU impact. However, the extension rules propose that to qualify for MLIU impact, patients can be either low-income or uninsured.
Provider impact and considerations:
This expansion to include patients that are Medicaid, low-income or uninsured should make it easier for providers to hit their MLIU targets (more patients qualify for the MLIU umbrella). Still, there is additional work because providers must alter their reports and calculations of MLIU impact to account for this change. Outreach programs that target MLIU patients specifically should also change their workflows and strategies to account for a larger patient population.
Proposed change: Transition to four standard milestones in Category 1 and 2
Under the transition year, HHSC proposes that each Category 1 and 2 project have the following four milestones: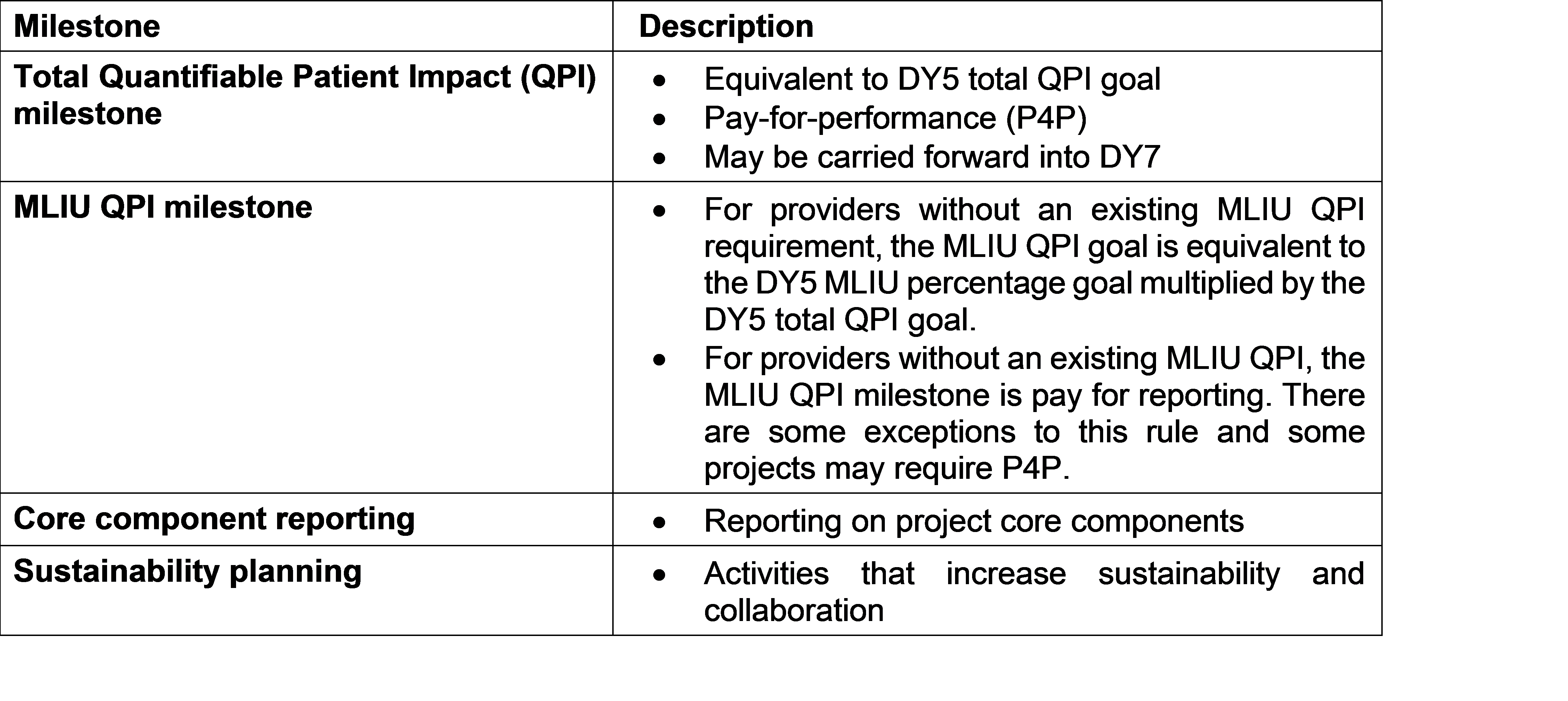
Each of the milestones is worth 25 percent of each DSRIP project’s Category 1 or 2 value.
Provider impact and considerations:
With the new Category 1 and 2 goals, providers will need to reexamine their DY6 projected achievement dollars based on past performance. The core component reporting and sustainability planning milestones are process milestones, which should be relatively straightforward to achieve. The Total QPI milestone remains a pay-for-performance goal, but most providers will have pay-for-reporting MLIU QPI milestones (depending on qualifying factors). These changes shift much of the dollar risk from P4P to pay-for-reporting (P4R) in the transition year, which is beneficial for providers.
Providers should analyze their past and current performance in hitting their MLIU goals to prepare for the possibility of P4P on MLIU targets. The MLIU QPI milestone may or may not be tied to payment depending on certain factors, including past performance on MLIU targets (projects that have not been hitting their QPI percentages may be required to have P4P MLIU milestones in the transition).
The proposed rules also contain a provision to allow providers to request an adjustment to their MLIU goals. Providers should be prepared to request adjustments if they anticipate their MLIU goal will be P4P.
Additionally, providers should begin to conceptualize what sustainability activities they will want to pursue in the transition year.
Proposed change: Opportunity for project replacement; evaluation not part of Category 3 funding
With the waiver renewal, HHSC has indicated that providers will have the opportunity to replace projects, but that they must continue the current projects into the transition year to be able to retain the value in the renewal. In contrast to previous updates, however, HHSC has indicated that Category 3 funding in DY6 will not include project evaluation funds. Given the uncertainties around project replacement and evaluation, providers should still independently conduct an evaluation of their projects to prepare for success in the waiver renewal after the transition year.
Provider impact and considerations:
The Category 1 or 2 project-level evaluation is an opportunity to determine whether providers would like to continue or replace projects in the potential waiver renewal. This is a chance for providers to evaluate the success and alignment of their projects. Providers can take this opportunity to decide whether they should discontinue a project that has not been achieving the desired outcomes or no longer fits into the organization’s strategic goals, replacing it with a project that is more aligned with the provider strategy and operations. COPE Health Solutions has experience in strategic planning and initiative alignment, including DSRIP-related evaluations. For more information, see our other digest article: Preparing for the Texas 1115 Waiver Renewal – DSRIP Project Sustainability vs. Project Replacement.
Proposed change: Continued compliance monitoring
HHSC continues to reserve the right to subject providers and plans to potential audits from an independent assessor, similar to the ongoing Meyers and Stauffer reviews of project progress.
Provider impact and considerations:
Providers must continue to document activities and archive all past documentation of project achievement. Providers are encouraged to develop a strong knowledge management process or platform as this requirement will be relevant throughout the waiver renewal (another five years).
Bridging the Gap
COPE Health Solutions has deep expertise in clinical redesign and business requirements development for population health and integrated delivery systems. We understand the complex Medicaid waiver implications for health system lead agencies and partners. Our team has unparalleled experience and a proven track record of successes from planning to implementation to measurement with 1115 Medicaid Waivers in New York, Texas and California. Our subject matter experts can help your system move toward its long-term strategic goals, using the waiver as a path to success.
For more information about how COPE Health Solutions is helping clients across California, New York, Washington and Texas prepare for waiver changes, please contact: dsrip@copehealthsolutions.com.