 Providers in California, Texas and New York are currently implementing transformation projects under various 1115 Waivers to achieve the Quadruple Aim: better health, better care, less cost, higher satisfaction. Work under delivery system reform incentive payment programs (DSRIP) — the component of 1115 waivers that pays for outcomes if providers change practices from volume to prevention and value — is not for the faint of heart. Most states implementing transformation projects have created regional entities tasked with coordinating projects across newly built networks created for the purpose of the waiver program. Local coalitions are key to the successful implementation of Medicaid transformation projects and eventually drawing down the waiver funds.
Providers in California, Texas and New York are currently implementing transformation projects under various 1115 Waivers to achieve the Quadruple Aim: better health, better care, less cost, higher satisfaction. Work under delivery system reform incentive payment programs (DSRIP) — the component of 1115 waivers that pays for outcomes if providers change practices from volume to prevention and value — is not for the faint of heart. Most states implementing transformation projects have created regional entities tasked with coordinating projects across newly built networks created for the purpose of the waiver program. Local coalitions are key to the successful implementation of Medicaid transformation projects and eventually drawing down the waiver funds.
These regional coalitions usually include representatives from different sectors needing to participate in population health management (care delivery, public health, social services, government, etc.). In Washington, nine regional entities called Accountable Communities of Health (ACH) were developed under a Center for Medicare and Medicaid (CMS) Innovation grant to transform care in the state. These ACHs bring together key stakeholders in an effort to increase access to integrated, comprehensive, member-centered population health management and care services. ACHs are establishing a new leadership paradigm, in which health care is helping to drive community-wide changes for population health improvement.
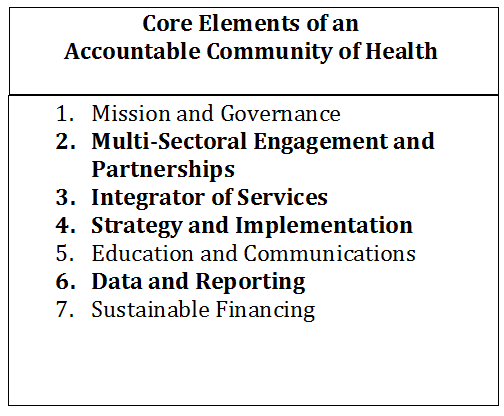
The Prevention Institute outlines seven core elements of an ACH; we will discuss how core elements 2) Multi-Sectoral Engagement and Partnership, 3) Integrator of Services, 4) Strategy and Implementation and 6) Data and Reporting relate to the potential requirements of the 1115 waiver. The information presented in this article is based on past experience with waivers in other states – the waiver in Washington has not yet been approved by CMS and the rules have not been finalized or announced.
Multi-sectoral Engagement and Partnerships
ACHs are regional collaboratives that bring together public and private entities to form multi-sector partnerships that work on shared health goals to incorporate social determinants of health in all aspects of health transformation. It is a contractual requirement of ACHs that their governance includes cross-sectoral involvement. These are relationships that have not been encouraged in the siloed system of care that centered around providing care in the hospital setting. Providers and payors are starting to acknowledge the significant role that social determinants of health (housing, food, transportation, income) have on the eventual outcomes that were being treated in the acute care setting. Tribal engagement is also strongly encouraged. The purpose of the ACH is to formalize relationships across the care continuum and leverage them to transform care.
ACHs need to formalize expectations and legal commitments to ensure service continuity among providers who are either competitors (providers, health plans) or are not part of the Medicaid delivery system (community organizations: housing, food, transportation, behavioral health). The 1115 Medicaid waiver presents an opportunity to receive incentive payment for this work and define the requirements in the initial stages. ACHs can implement a phased engagement approach tailored to the local environment that brings the voice of consumers and individual community members to ACH development and decision-making. The first step is engaging partners who are willing to collaborate or come to the discussion table to shape the health of their community. Creating workgroups, steering committees or other opportunities for regular sharing of ideas and lessons learned is key to keeping stakeholders engaged. Additionally, the incentive of the 1115 waiver should be used to bring partners together.
Table 11
Integrator of Services
Similarly, to the core element of multi-sectoral engagement, the end goal of the ACH effort is to create integrated delivery systems that are aligned in incentives and payment methods. This requires creating a system around the “whole person” that addresses physical and mental health through addressing social determinants of health as well as treatment for illness or injury.
This whole person approach should integrate disparate community services that address social determinants of health, ACES and trauma-informed mental health care with traditional Medicaid benefits. Integrating these services drives the Quadruple Aim outcomes of better care, better quality, lower costs and more satisfied providers. The advanced step after multi-sectoral engagement is actually creating integrated networks on the relationships built. This includes identifying best-fit partners, assessing capabilities and willingness to collaborate long-term, defining requirements and desired outcomes/incentives, and creating formal contracts for service or outcomes. Legal partnerships support statewide payment systems that reward positive outcomes and guide reinvestment of potential savings into prevention and early intervention services.
The ACH framework develops the “single door for access” regional service model by providing access to comprehensive integrated services. This will change the structure and incentives of the current health care system.
Strategy and Implementation
Much of the responsibility of an ACH is defining the strategy of the region in regards to health care transformation. The ACH framework supports the planning and decision-making authority needed for transformation projects and for population health implementation. Based on preliminary waiver rules, it appears that ACHs will decide which transformation projects to pursue under the 1115 waiver and should make those decisions based on regional community health needs assessments. Incorporating stakeholder engagement, the ACH will need to prioritize which health and community issues are short-term, mid-term and long-term goals for the community.
Beyond planning, the ACH will oversee the implementation and performance risk for projects and will monitor the quality improvements and value-based targets for reimbursement. It may be responsible for reporting on 1115 waiver projects to the state and determining the funds flow down to providers, although the final waiver rules have not been determined and this assumption is based on past waivers in other states.
Data and Reporting
Data and reporting is a major component of 1115 waivers and DSRIP-like programs – you cannot earn incentive funds without first demonstrating that you have achieved the outcomes. And these reports are subject to audits, which means that providers must demonstrate in good faith that their data is reliable, accurate and comprehensive. Tying this in with the movement toward integrated delivery systems across a variety of partners, it is easy for data collection to become muddled in issues of interoperability and defining the populations.
ACHs must take a leadership role in defining data requirements and data quality standards. It should also take the lead in developing solutions to address 1) partners that are not on systems that can collaborate or share data and 2) partners who are not using electronic medical records or who do not historically track data on their clients (food banks). Solutions include continuing to increase the functionality and bi-directionality of regional health information exchanges or working with payors to access claims data for a comprehensive health picture (both New York strategies currently). States such as Texas and California are continuing to focus on internal data collection capabilities through upgrading population health capabilities in their medical records system or beefing up their data analytics resources.
How can COPE Health Solutions help you with planning and implementation?
These core elements are critical areas that drive the longer-term success and viability of the role of ACH’s. They must demonstrate how contractual and financial levers are used to sustain community reinvestment and sustainable incentive structures that can last well beyond the waiver. This approach ensures mutual accountability for the performance of the health system in service of whole-person health.
COPE Health Solutions is a leading national health care consulting firm with extensive experience with 1115 waivers. With offices in California, New York and now Washington, COPE has assisted our clients with successfully assessing, planning and executing transformation projects in multiple states. Our clients include but are not limited to the Finger Lakes and Mount Sinai Performing Provider Systems in New York to Central Health in Texas and Kaiser Permanente in California. For more information, please contact info@copehealthsolutions.com.
Footnote:
1www.preventioninstitute.org