
The year 2017 is upon us, and that means that the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015 is in effect for eligible clinicians who participate in Medicare Part B. MACRA is a bipartisan approach to physician payment reform attempting to repair the patient-provider relationship, as the Centers for Medicare and Medicaid Services (CMS) hopes that the legislation eases provider burden on documentation and paperwork – allowing them to focus on quality and efficient care to the patient.
The final MACRA rule, released in October of 2016, is over 2,100 pages long. The program is complex and will change from year-to-year. CMS is referring to 2017 as the “transition year” and has provided eligible clinicians1 options to pick their level of participation for the Merit Based Incentive Payment System (MIPS) or advanced Alternative Payment Models (APMs) which are the two programs that constitute the Quality Payment Program (QPP). CMS has launched a website2 that provides a high-level overview of MACRA and its programs along with numerous resources for those interested in learning more.
While eligible clinicians are those who are required to participate in the QPP, implementing MACRA will impact health care administrators, practice management, information technology (IT) staff and vendors at a minimum. This Health Insights article will examine the following five items your system or independent practice association (IPA) should focus on early in 2017 and throughout the year to ensure your overall success with MACRA requirements, and secure a neutral or positive payment in 20193.
- Education and governance
- Review historical performance and institute a change management program
- Develop a roadmap for 2017
- Partnering with your electronic health record (EHR) vendor
- Cultivate a strategy/plan to graduate from the MIPS track to Advanced APMs
COPE Health Solutions’ versatile team is equipped to assist systems and IPAs with these critical elements of preparation and looks forward to opportunities to partner with organizations to transition these items from theory to reality.
1. Education and governance
According to a recent study by The Physicians Foundation4 “only 20 percent of physicians are familiar with MACRA” and its components. As of January 1, 2017, MACRA participation is required and providers and practice managers need to be concerned about the level of education their providers and support staff have regarding the QPP and its impact on future payment. Furthermore, while MACRA is currently only a Medicare program, it is likely that Medicaid and private payors will adapt similar reimbursement strategies in the near future. Systems and IPAs should invest time and resources to ensure that their providers and support staff understand what will be required in 2017 and later years, and how this will impact their day-to-day work, payments and experience with patients and other providers. It will be important for providers to understand how their individual performance will impact the larger group practice and to inform them that their performance will be published on Physician Compare, where patients will be able to compare and contrast the performance of doctors and groups (which may impact where they decide to seek care).
One key to success will be to ensure that providers have a voice at the table and are part of the decision making regarding strategic decisions that will need to be made as part of participation in the program. Systems and IPAs should consider forming a multidisciplinary steering committee if they have not already that is focused on the implementation of the QPP. This group should be comprised of clinicians, management, IT and support staff and should be charged with overseeing the work that will be required for initial success. The steering committee should focus on key tasks such as selecting quality measures, reviewing data collection and reporting workflows and capabilities, restructuring current workflows to ensure performance with QPP standards and requirements, further training and education and ultimately oversee performance monitoring and develop quality improvement strategies. It is also imperative to educate all physicians on the importance of participating in a qualified clinical data registry (QCDR) to adequately report MIPS performance metrics. Each specialty society should be contacted in order to participate in these data registries.
COPE Health Solutions can assess your clinical and administrative teams’ current understanding of MACRA and its implications on care delivery and payment. From there, our firm can partner with your team to develop an educational training approach that meets your organizations needs and work with you to ensure that your entire team is informed and able to move forward with the next steps ensuring success under the QPP.
2. Develop a roadmap for 2017
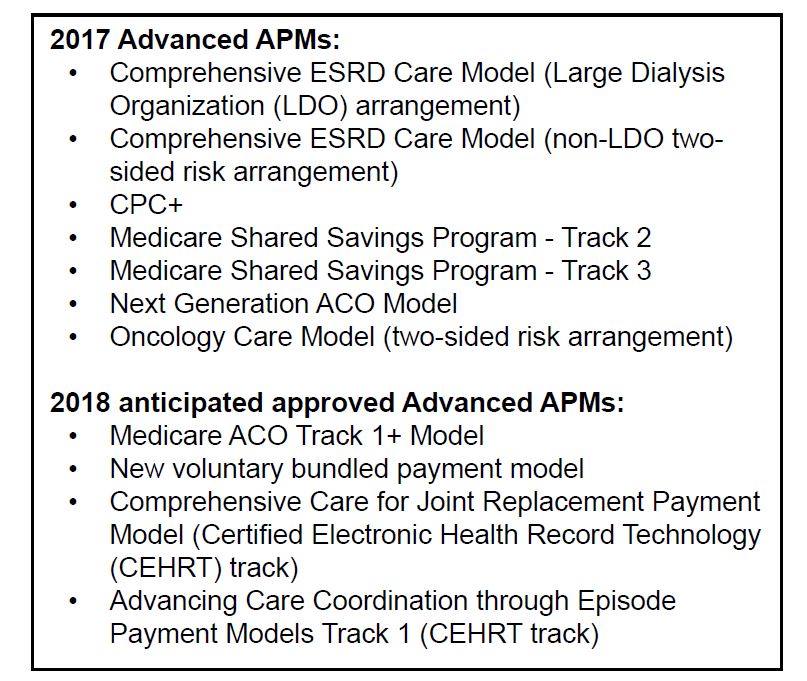
Physicians, either individually or in groups, will participate in the QPP either through the MIPS or Advanced APM tracks. In order to participate in an Advanced APM, eligible providers (EPs) must already be participating in an approved model for the 2017 year. To earn the 5 percent incentive payment for 2019, providers must not only have already participated in Advanced APM but further receive 25% of their Medicare Part B payments through the Advanced APM or see 20% of their Medicare patients through the Advanced APM2. For the 2017 performance year, CMS estimates that only 70,000-120,000 of the 600,000+ clinicians who will be impacted by MACRA will have participated in Advanced APMs5. Each year, CMS will release new opportunities for qualifying Advanced APMs for clinicians.
Organizations who are not eligible to participate in the Advanced APM are automatically required to participate in MIPS. In their effort to encourage 100% participation, CMS has provided MIPS eligible clinicians the opportunity to “pick their pace” — or level of participation — for 2017 in order to avoid a negative adjustment to their 2019 payment. CMS has provided three options for clinicians for 2017: testing, partial and full participation2.
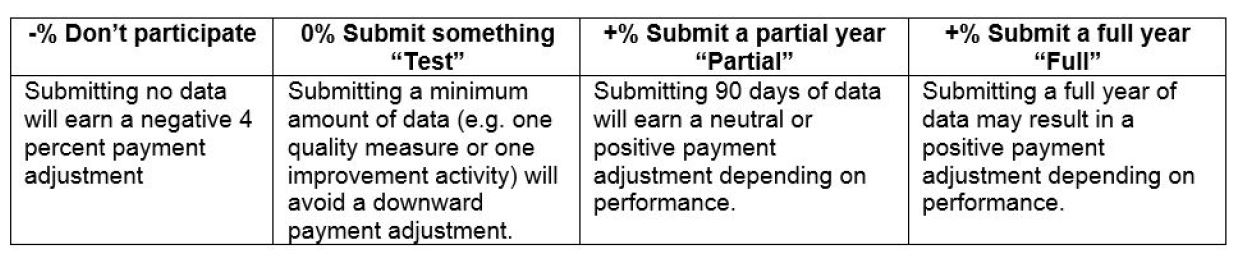
Utilizing the steering committee, systems and IPAs can determine what level of participation makes the most sense for their organization and prepare their activities for 2017 based on this decision. Even at the lowest level of participation, submitting the minimum amount of data, organizations will have to agree on at least one quality measure or improvement activity to focus on and report in 2017. With over 270 Quality Measures, 15 Advancing Care Information objectives and 92 Improvement Activities for the 2017 reporting year, there will be a large amount of information to consider when selecting which activities systems or IPAs will measure and report on for 2017. Organizations should select measures and activities that directly apply to the type of care their clinicians practice, measures they have the ability to collect and report data on, and have a strong opportunity to improve their performance in these areas in order to set themselves up for the most success in the first year of the QPP. CMS will not include cost metrics in the final 2017 MIPS score. Thus, it will be critical to review CMS’ feedback throughout the 2017 performance period to analyze future cost scores.
After assessing the organization’s understanding of MACRA, COPE Health Solutions can work with you to develop a strategic roadmap for 2017 and 2018, assisting with the development of a steering committee and equipping key leaders with the right information to make the decisions for what path makes the most sense for your early success in the QPP.
3. Review historical performance and institute a change management program
CMS is prepared to provide feedback on 2017 performance in 2018, but that leaves little room for providers to understand how their 2019 payment may be impacted in real time. One of the best things systems and IPAs can do in early 2017 is understand their past performance in other CMS quality programs. The MIPS track of the QPP combines three past reporting programs: the Physician Quality Reporting Program (PQRS), the Value-based Payment Modifier (VM) and the Medicare Electronic Health Records (EHR) Incentive program (or Meaningful Use). It also introduced a fourth element known as the Clinical Practice Improvement Activity. Streamlining these old programs provides systems and physician groups the opportunity to review their historical performance under these programs and identify key areas to focus on change management to increase performance in the first reporting year under MACRA. For organizations who participated in PQRS, they can access their PQRS feedback through CMS as well as their performance under VM through their Quality and Resource Use Report (QRUR). Utilizing past performance to enact a change management strategy will be important, along with strong leadership to initiate and maintain quality improvement efforts achieved under either track of the QPP (MIPS or Advanced APMs). Organizations can leverage their steering committee for leadership and strategic direction regarding where to focus change management efforts to improve key aspects of their practice.
After helping define the plan for 2017, the COPE Health Solutions team will work with you to understand current performance as a group or by individual providers and identify the areas where your organization should focus your change management efforts. Our firm has experience in assisting organizations with initiating change management initiatives and developing or improving project management offices to ensure long-term success with change management efforts.
4. Partner with your EHR vendor
A robust and flexible EHR will be critical to success under MACRA for systems and IPAs. Even for organizations who have meet past Meaningful Use (MU) measures, requirements under MIPS expect organizations to have advanced IT capabilities for not only reporting and analytics but also interoperability between physicians to exchange information and increase their use of data registries. Organizations can check to see if their current EHR is ready for the transition from MU to MIPS by using the Office of National Coordinator for Health Information technology (ONC) look-up tool6. It will be important to work with your vendor to ensure your reports can be used both for MIPS reporting and population health efforts in your practice, and that these reports can be easily run and accessed by members of your internal IT team. You may need to work with your vendor to identify upgrades to your system or provide continued training. EHR product support of new payment model adoption is critical, and Certified Electronic Health Record Technology (CEHRT) will determine success in reporting in 2017 for MACRA. A careful security risk analysis in 2017 with your EHR vendor will advance practice groups in having MACRA success.
COPE Health Solutions can partner with you to identify key questions and activities you may need to engage your EHR vendor in early in 2017 to be successful under the QPP.
5. Cultivate a strategy/plan to graduate from the MIPS track to Advanced APMs
For some organizations a desire to participate in Advanced APMs may lead their long-term strategy for maturing their clinical practice and lead them to take on risk for the population they manage. Participating in an Advanced APM means that systems or IPAs have taken steps beyond the requirements of MIPS to deliver efficient, high-quality care while taking on downside risk. Overall, Advanced APMs offer more potential rewards for clinicians than the MIPS track. For example: a higher fee schedule in 2026 and beyond in addition to the 5 percent lump sum bonus payment for participation in approved models come with greater risk if required savings are not realized. Advancing from MIPS to Advanced APMs means meeting standards to apply for an Advanced APM that is recognized by MACRA and taking applications to perform standards for the measurement year to receive incentive payments. This decision and hard work to advance to this level of care delivery and risk will take leadership and physician buy in, support from all staff, IT capabilities, and redefined contracts inclusive of risk at a minimum to be successful. While daunting, organizations who participate and perform well under Advanced APMs will lead the health care community as some of the elite few who have truly mastered value-based payment and care delivery.
COPE Health Solutions has a proven track record of success taking our clients from strategic planning to implementing initiatives working alongside our clients step-by-step, providing tailored market-relevant solutions that complement our client’s unique skills and capabilities. Our firm will apply our knowledge and skills to assist your system or IPA in the decision making and strategic plan to participate in Advanced APMs, if that is right for you.
About COPE Health Solutions
COPE Health Solutions is a nationally recognized firm with the vision, knowledge, and skills to help your organization set a course for success under MACRA regulations both within MIPS and Advanced APMs. Our team is comprised of experts in value-based payment contracting and key population health management systems. Partnering with us to analyze your readiness for MACRA and the Quality Payment Program will be a rewarding first step for your system or IPA during the critical first year of the program. Please contact us at info@copehealthsolutions.com to learn more.
Thanks to Harut Hovsepyan, MD, for contributing to this article.
Footnotes:
1 Physicians, PAs, NPs, clinical nurse specialists, certified registered nurse anesthetists
2 http://qpp.cms.gov/
3 Participation and reporting in 2017 will impact 2019 provider payments/ adjustments
4 http://www.physiciansfoundation.org/uploads/default/Biennial_Physician_Survey_2016.pdf
5 https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2016-Fact-sheets-items/2016-10-25.html
6 https://chpl.healthit.gov/#/search