Overview
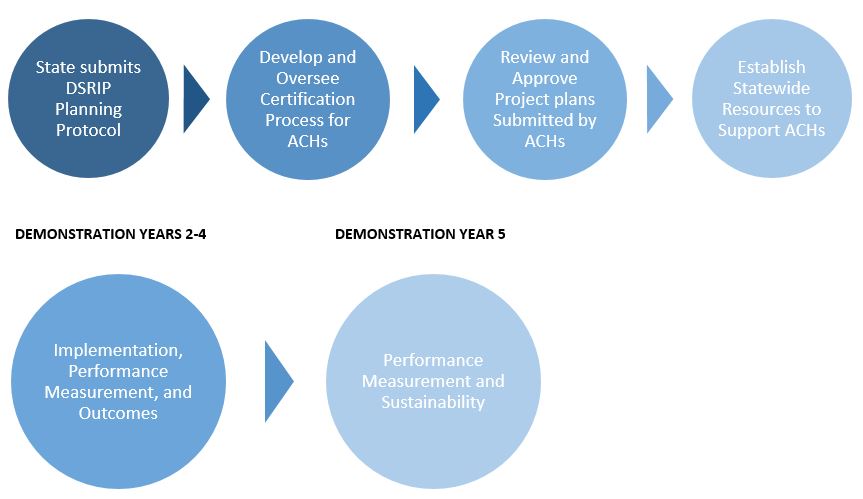
On January 9, 2017, Washington State Health Care Authority (HCA) released highly anticipated Special Terms and Conditions (STC) outlining the provisions of the Section 1115 Medicaid demonstration waiver. The five-year waiver is active now through December 31, 2021. Under this demonstration, a delivery system reform incentive payment (DSRIP) program aims to increase access, improve health outcomes and increase the quality of care among Medicaid beneficiaries by prescribing a menu of innovative regional transformation projects. The DSRIP program authorizes Accountable Communities of Health (ACHs) to coordinate and oversee the regional projects focused on building health system capacity, care delivery redesign, prevention, and health promotion and preparing for value-based payments. These ACHs are being used as a vehicle to fulfill Washington’s commitment to adopting alternative payment models (APM) that align with DSRIP goals focused on improving quality and cost of care by converting 90 percent of all Medicaid provider payments by 2021.
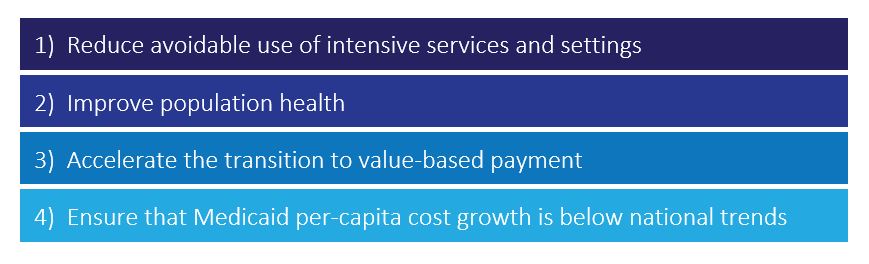
High-Level Waiver Goals
Connecting the Dots
ACHs will tie together the waiver requirements and CMS aims by means of contracting, plan writing and reporting. During the first months of the demonstration year, ACHs will become incorporated as LLC or nonprofit entities and will develop networks aligned with Washington’s regional service areas for Medicaid purchasing. Each ACH will be responsible for outcomes determined by Medicaid beneficiaries residing in respective service areas. It is critical that ACHs develop comprehensive project plans with an appropriate selection of projects to assure they are well positioned for success during the five-year demonstration period, as clinical outcomes associated with each project are tied to value-based payment structure and goals. Project plans will be developed using guidance from the state planning protocol and will require ACHs to solicit community feedback prior to the submission of the project plan to ensure the needs of the region are being met. Community needs, informed by a Regional Health Needs Inventory (ACH-tailored community needs assessments), will drive project selection and ultimately performance requirements. Each project goal or objective will have an associated outcome metric that will be reported in all years of the demonstration with baseline data for all applicable quality improvement and outcome measures to be included in initial project plans. Depending on how baseline collection is defined by the state, the data collection required to obtain this data could be a large challenge in submitting project plans in time.
MCOs as Key Stakeholders
Central to the Washington State DSRIP model is the role managed care organizations (MCOs) play as stakeholders. These organizations must be heavily involved as the shift to value-based payment is a key component of the transition plan after the demonstration period is over. MCOs are expected to sustain changes made to the delivery system and ensure business approaches adapt to new models of care delivery. These entities will participate in the design and implementation of delivery system reform projects as well as actively provide leadership or supportive capacity in every ACH and collaborate with provider networks to implement value-based models. Although MCOs will not receive any incentive payments, the state will set aside up to 15 percent of annually available DSRIP funds to reward high achieving MCO and ACH partnering providers for the provider-level attainment of value-based payment targets.
DSRIP Funding
Washington State is authorized under the DSRIP program to claim up to $1.125 billion over the five-year demonstration period in the form of performance-based incentive payments. The Program Funding and Mechanics Protocol (PFM) should be developed sixty days after the STCs were approved, and they were approved on January 9. The PFM will determine an allocation formula to be used across ACHs based on covered Medicaid lives per ACH, the scale of the project, type of project, level of impact on beneficiaries and number of providers, amongst other factors. Beginning in demonstration year 3, up to 5 percent of annual DSRIP funding will be at risk if the state fails to demonstrate progress toward meeting the demonstration’s value-based payment goal (which is 90 percent of Medicaid provider payments rewarding outcomes instead of volume by 2021). This amount jumps to 10 percent in demonstration year 4 and 20 percent in demonstration year 5, resulting in almost $40 million at risk for performance. The state hopes to incentivize partners and stakeholders to work together to develop a system that thrives under alternative payment models. Within 60 days of demonstration approval, the state is mandated to release a value-based payment roadmap to guide partners and providers by setting targets for value-based payment attainment and providing a description of how managed care is transforming to support new models of care. The roadmap will be updated annually at the beginning of each demonstration period.
Life Cycle of the Five-Year DSRIP Program
About COPE Health Solutions
COPE Health Solutions is a national health care consulting firm that advises hospitals and health care systems on strategy, population health management, Medicaid waivers, and workforce development solutions. COPE Health Solutions provides clients with the tools, services, and advice they need to be leaders in the health care industry. We understand the complex waiver implications for health system lead agencies and partners. Our team has unparalleled experience and a proven track record of success from planning to implementation to measurement with 1115 Medicaid Waivers in New York, Texas, and California. Contact info@copehealthsolutions.com to learn more.