Introduction
Social determinants of health (SDOH) can play a major role in ensuring better health outcomes at both the individual and population level. SDOH are responsible for over 80 percent of health outcomes while clinical interventions represent only 20 percent1. While the impacts of SDOH are well known, many providers and organizations still do not know or understand the specific drivers outside of the hospital, ambulatory and post-acute settings that influence the health outcomes of the patient population they manage. Collecting and understanding these non-medical drivers is critical in helping providers and health organizations improve care for the populations they serve.
Although the general practice of data collection in health care has improved in recent years, a standardized method of collecting data, specifically for SDOH, across providers has not been identified and organizations have struggled to find meaningful use for the data gathered to drive patient-centered care. Additionally, the health systems and providers that do collect useful data often gather the information in unstructured and unusable formats.
A focus on improving the data collection methods precisely for SDOH and targeted patient intervention must become a priority for health care organizations moving forward. The data collected provides actionable insight and valuable information required for patient stratification and innovative initiative design. These initiatives can address not only the issues occurring within the hospital walls but also drivers outside the hospital that contribute to the patient’s overall health outcome and status.
Improving uniformity in the data collection process, effective collaboration and aligned incentives among key stakeholders on the method SDOH data should be gathered, shared and used as these are important to driving initiative development and deployment. This approach will in turn lead to healthier outcomes from targeted patient-centered care. This article examines the current state of SDOH data collection and provides recommendations on how to improve the process for SDOH data collection to help better achieve the Triple Aim goals.
Current State of SDOH Data Collection
The accurate capture of SDOH information is challenging due to a lack of agreement on standard assessment tools, data sources, measurable inputs and best practices on tool implementation across the industry. Progress made in data collection is further hindered by a general lack of knowledge and consensus for sharing best practices, struggles, successes or failures and as well as a lack of effective collaboration between providers, community-based organizations (CBOs), managed care organizations (MCOs) and other health organizations.
As a result, providers do not adequately understand the factors that influence roughly 80 percent of their population’s health outcome.
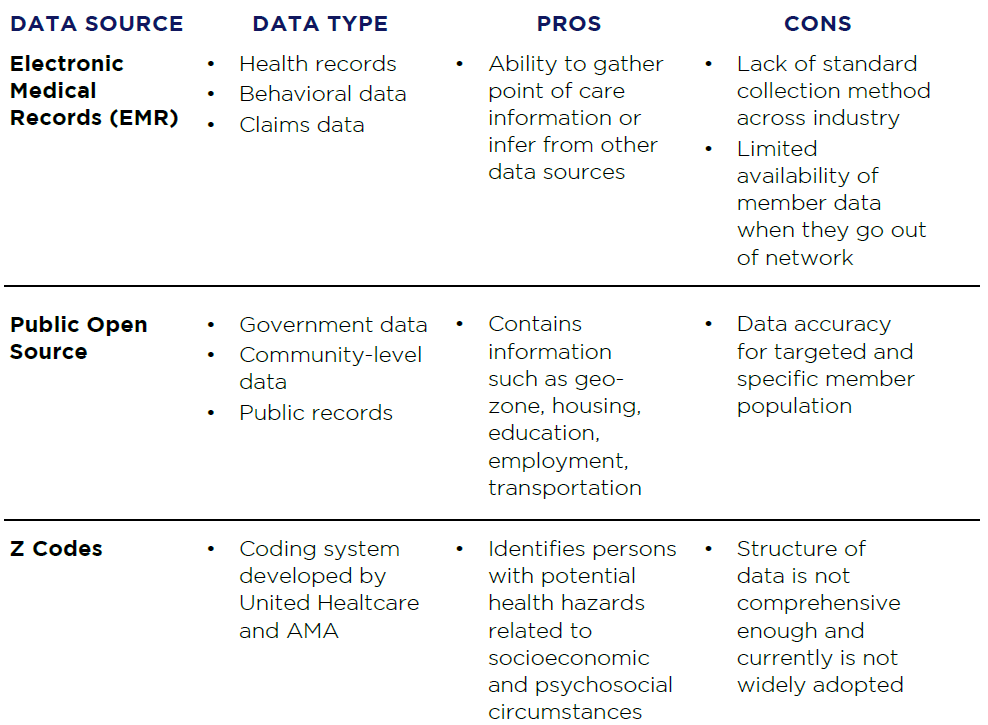
The table on the next page shows the current state of data sources, along with the pros and cons:
Table 1: Pros and Cons of Current SDOH Data Sources
Improving Data Collection for the Right initiative
The following recommendations will help improve data collection for SDOH and develop initiatives for patient-centered care:
1. Build Effective Collaboration Between Multiple Sector Stakeholders
- Multi-stakeholder collaboration to improve SDOH data collection.
Stakeholders across multiple platforms and industries must work together to develop the right process and protocol to collect, share and handle data. This includes private health and technology sectors working together with the state and federal government, among others, to develop and streamline the most effective data collection process, framework and methodology for SDOH. MCOs are taking a more active role in this space and partnering with social referral platform vendors such as NowPow, UniteUs and Aunt Bertha to leverage non-medical systems. This can be a key opportunity for collaboration across stakeholders. - Address and involve health in non-health sectors.Integrating non-health sectors into the brainstorming and decision-making around social determinants of health helps to challenge the status quo and infuse new innovations and policies.
This in turn fosters better collaboration among multiple stakeholders with the aim of improving data collection accuracy. Recent trends in private equity are challenging organizations to include building SDOH into underwriting and introducing more non-medical factors into the equation to help improve clinical outcomes and reduce total medical spend. - Community engagement.
An important and effective way to improve the accuracy of data collection and patient-centered care is to engage the community, particularly with CBOs. Organizations strategically collaborate with local stakeholders and obtain their input, participation and insights to further understand their social needs. This approach not only improves the collaborative partnership between local communities and their respective health organization but also helps providers understand the data points necessary for creating the most optimal framework. Understanding the key information CBOs collect and have access to should be taken into consideration when developing SDOH data strategies.
2. Standardize data source and tools for impactful use
- Developing the right set of requirements
Payors and providers must establish or clarify how they intend to use the SDOH data and how it will influence their organization’s overall strategies. Setting the right requirements will help inform organizations on how to develop the appropriate processes, as well as, assist in the design of the right workflow for patient-centered care. This approach, with the use of the right screening, assessment, and analytic tools, will drive actionable insights and lead to opportunities to collaborate with CBOs to drive a more holistic person approach to care management.The next step to consider would be the use of an analytic platform that integrates SDOH data with other member information from sources like claims data to further understand the financial impact of these member cohorts. - Data validation for impactful use
Validating the information collected from patients is important to improve the overall data collection process and should be conducted at every point of care, similar to the medication reconciliation process. Once the initial SDOH information is received, the data gathering process should transition from obtaining patient social and welfare information to validating the information collected in a standardized manner to ensure it is reportable and can be easily analyzed in the future. This validation process is critical to integrity of the data especially when sharing it with other sectors of the industry such as health plans that are also key stakeholders in contributing to the Triple Aim. - Improve the adoption of standard available codes
Currently, Z codes are the industry-standard SDOH codes available for financial reimbursement. These codes can be used in the reporting of factors influencing health status (SDOH) for which standard medical codes are not adequate. Unfortunately, these codes are not yet widely adopted as they are mostly utilized for reimbursement purposes. The codes already existing should be improved to help capture SDOH data more accurately, improve reimbursement methods and help in patient-centered initiative design industrywide. Until that happens, organizations can educate themselves about Z codes and build the use of them into their workflows. The more standardized ways of collecting non-medical information that are put into action today, the more actionable information the industry will have in the future.
3. Develop and adopt appropriate metrics and dashboards for valuable insights
- Use metrics to track quality and outcomes in executive, management and care management dashboards.
As the right performance indicators and metrics are developed, they should be used to track the quality and outcome of the care provided in dashboards used to track performance across the care and payment continuum. In fact, the success of a patient-centered initiative can only be determined when the right performance indicators and metrics are tracked. Examples of non-medical interventions that can indirectly impact health outcomes such as HEDIS and NCQA measures include the number of timely appointments a transportation provider made each month or the number of members who received “prescriptions” for healthy food at a local food bank or grocer. Organizations should set key performance indicators (KPIs) that can evaluate and track this information and help link the interventions to overall health outcomes. - Design the right dashboards for patient-centered care.
The ability to translate data into a format that is understandable and visually appealing is essential in the grand approach to patient-centered care. The format and dashboard should capture the relationship between different SDOH categories and chronic diseases/hospital services utilization. These dashboards will help providers approach patient care with valuable insights because of the data-driven approach behind these developments. Dashboard designs should ensure the patient care approach is all-encompassing, factoring issues that affect patients inside and outside of the hospital, in the clinic or in post-acute care setting walls.
While conflicts and challenges remain among stakeholders on how to approach using SDOH data, the recommendations above can help traditional healthcare organizations, and their community based organization partners, to challenge the status quo and help drive transformation around building in the non-medical attributes of whole-person care.
Regardless of the potential challenges, providers, payors, community based organizations and other key stakeholders must constantly push for improvements in the standard collection and use of SDOH data, as the improvement and standardization of data collection will enable targeted interventions for patients and improve outcomes.
For more information on how to improve the collection of your SDOH and leverage it to drive better patient outcomes, please contact Yomi Ajao at yajao@copehealthsolutions.com or 636-793-1873. Mr. Ajao is Senior Vice President at COPE Health Solutions and President of Analytics for Risk Contracting, LLC, a SAAS platform that enables healthcare providers to determine their actual care costs and understand the net financial effect of specific care improvement efforts, population health management and other quality and cost initiatives by leveraging data from multiple sources, including claims and SDOH data.
Endnotes
1 https://www.redoxengine.com/blog/data-enabled-strategy-for-the-social-determinants-of-health/
2 https://healthpayerintelligence.com/news/using-social-determinants-of-health-for-risk-stratification
3 https://dashconnect.org/wp-content/uploads/2016/06/Using-Social-Determinants-of-Health-Data.pdf
4 https://www.who.int/social_determinants/sdh_definition/en/
5 https://www.pwc.com/gx/en/healthcare/pdf/pwc-social-determinants-of-health.pdf
6 https://healthitanalytics.com/news/icd-10-allows-non-physician-documentation-of-social-determinants
7 https://www.fortherecordmag.com/archives/0517p14.shtml
8 https://tincture.io/at-a-glance-new-z-codes-for-sdoh-c8b2260e0fe3
9 https://www.kff.org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/
10 https://www.urban.org/research/data-methods/community-engagement-methods-urban
11 http://www.healthdata.org/social-determinants
