California public hospitals have a unique opportunity to leverage the PRIME program to help build the competencies needed to thrive in a risk-based environment. Public health systems and hospitals that make strategic investments in data analytics, network optimization, care management and quality improvement will be set up for success and long-term sustainability.
Overview
The Centers for Medicare and Medicaid (CMS) approved the most recent 1115 Medicaid Waiver in California in January 2016. This extension allowed for continued public hospital participation in the Delivery System Reform Incentive Payment (DSRIP) program, now called PRIME, and introduced the participation of district hospitals. The extension was a challenge even under the Obama administration, and it is expected that under the current administration there will not be any future incentive payment program extensions in California.
The Medi-Cal 2020 waiver of $6.2B will end on December 31, 2020. For the past 13 years, California’s public hospitals have had access to waiver funds to expand beyond public hospital assets and build strong partnerships with community doctors, FQHCs, behavioral health organizations and long-term care organizations. With only three waiver years left, California public health hospitals must now navigate new State mandates to (a) contract with at least one Medi-Cal managed care plan in their service area by 2018 (Senate Bill No. 815) and (b) establish a pay-for-performance incentive payment program with applicable Medi-Cal managed care plans (Senate Bill No. 171). These are referred to as value-based payment (VBP) arrangements.
California’s Medi-Cal managed care benefits now include adult day health services, mental health services and, in seven demonstration counties, certain long-term services and supports. The inclusion of these high cost services, which have traditionally been carved out, represent new challenges and opportunities in a VBP contracting environment.
Requirements Post – Waiver
In accordance with these policy drivers, California public hospitals must harness remaining DSRIP funds to prepare for a post-waiver environment in which there will be less Medi-Cal dollars and more competition for managed care members.
 California public hospitals have a unique opportunity to transform into population health management systems and to maintain or expand market share for Medi-Cal. Another opportunity is growth of the Medicare population market share – particularly dual eligible and Medi-Cal members aging into Medicare.
California public hospitals have a unique opportunity to transform into population health management systems and to maintain or expand market share for Medi-Cal. Another opportunity is growth of the Medicare population market share – particularly dual eligible and Medi-Cal members aging into Medicare.
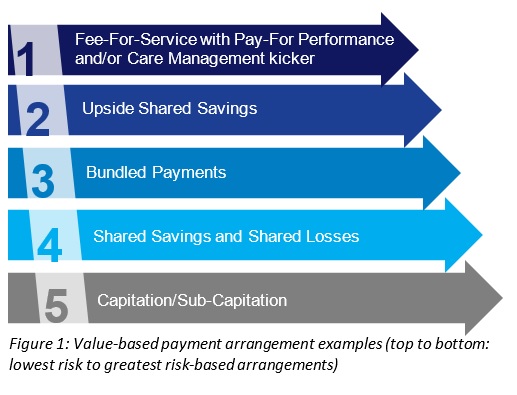
Transition toward risk is necessary for long-term financial sustainability of public health systems. Value-based payment (VBP) contracts between California Public Hospitals and Medi-Cal managed care plans will require the hospitals to bear some level of financial risk when delivering high quality care at low cost (see Figure 1 for types of VBP arrangements). Access to savings from reduced medical spend will mitigate the impacts of declining inpatient fee-for-service (FFS) revenue and Disproportionate Share Hospital (DSH) cuts. The evolution to risk should follow a gradual phase out of traditional revenue streams based on volume of services initially taking on upside only shared savings or FFS) with care coordination/pay-for-performance arrangements. This gives the organizations time to mature and build the infrastructure necessary to successfully reduce total medical spend per member while improving quality outcomes and provider satisfaction. Upon achieving this improved value, it is essential to consider ways of maximizing the return on investment, which include evolving contracts away from low-yield VBP arrangements and into full capitation.
Key Success Factors
When negotiating any VBP contract, key fundamentals should be considered. The kinds of arrangements health plans and providers are willing to enter depend on organizational readiness from an administrative, population health management and network adequacy perspective. This further emphasizes the need to reinvest PRIME dollars in population health management infrastructure.
 The move toward a successful value-based environment is embedded in functions that enable health systems to align payment with high quality care (Figure 2). As risk begins to shift from health plans to providers in managed care VBP arrangements, health systems should implement and optimize solutions that manage risk for attributed members. These functions may evolve from existing structures and programs developed under DSRIP / PRIME. Examples include community partnerships with well-defined CBO roles and payment methodologies, primary care access, care management and coordination, chronic disease management and other population-health improvement initiatives.
The move toward a successful value-based environment is embedded in functions that enable health systems to align payment with high quality care (Figure 2). As risk begins to shift from health plans to providers in managed care VBP arrangements, health systems should implement and optimize solutions that manage risk for attributed members. These functions may evolve from existing structures and programs developed under DSRIP / PRIME. Examples include community partnerships with well-defined CBO roles and payment methodologies, primary care access, care management and coordination, chronic disease management and other population-health improvement initiatives.
As with any strategic decision or new service, diligent planning must be undertaken prior to building core population health functions, including detailed cost modeling to estimate implementation and operating costs. Health systems must also self-assess roadblocks and cultural readiness to restructure, scale and redeploy resources. National/state and internal peer provider comparative benchmarks should be used to project profit and loss estimates using market-specific assumptions with relation to the ability to change provider, system and attributed member behaviors. Successful health systems should develop a phased transformation roadmap managed by a project management office and informed by claims, encounter and quality data analytics and modeling.
About COPE Health Solutions
COPE Health Solutions is a deeply mission-driven national health care consulting firm with expertise in health care systems strategy and population health management for clients across the health care continuum, including hospitals, health systems, physician organization and health plans. We remain deeply connected to our roots in homeless family outreach, education and health system navigation – lessons learned from this work guide us today. Our multidisciplinary team of health care experts have many decades of experience developing and managing health plans, IPAs, ACOs and population health management systems. They provide our clients with the tools, services and advice they need to plan for, design, implement and support successful operations in a rapidly evolving health care environment. To learn more about our expertise in population health and MSOs please contact info@copehealthsolutions.com.
