CMS CHART Model Fact SheetIn August 2020, the Centers for Medicare & Medicaid Services (CMS) announced Community Access and Rural Transformation (CHART) Model. This model is designed to support rural communities and providers in improving quality and access to care, while providing financial stability and upfront payments to support the transition to value-based payment models. The CHART Model offers two tracks: the Community Transformation Track and the ACO Transformation Track. While both programs have been announced together and target the same communities, the structure of the programs themselves are quite different from one another. Below, we take a closer look at the Community Transformation Track.
Community Transformation Track
CMS seeks to award up to 15 Lead Organizations with cooperative agreements of up to $5 million to administer a Community-wide Transformation Plan.
A variety of entities are eligible to apply to be a Lead Organization, including but not limited to:
- State Medicaid Agencies (SMAs)
- State Offices of Rural Health
- Local Public Health Departments
- Independent Practice Associations
- Academic Medical Centers
- Health Systems
These organizations will need to delineate the Community for the purposes of the program. A Community must encompass one or more counties or census tracts, each of which must be classified as rural, as defined by the Federal Office of Rural Health Policy’s grant program eligibility criterion. The Community must also include at least 10,000 Medicare Fee-for-Service (FFS) beneficiaries with a primary residence located within the Community.
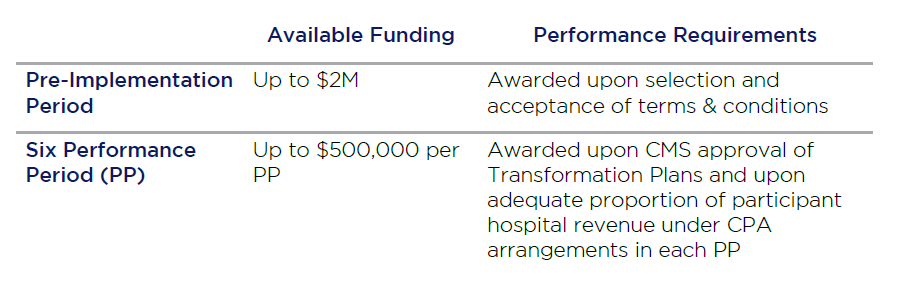
The Lead Organization will be the steward of the cooperative agreement funding. Disbursement of this funding is knotted to specific performance requirements. The program will span six performance periods and have a pre-implementation period. During the pre-implementation period, Lead Organizations will work with their community partners to develop a Transformation Plan which includes an assessment of the current state of the community as well as a full delivery and payment redesign strategy. During each of the six performance periods, Lead Organizations and community partners will work together to implement the Transformation Plan and meet milestones.
The funding for each specific Lead Organization will be disbursed through two mechanisms:
Each Lead Organization is required to form a cooperative that comprises at minimum an Advisory Council, Participant Hospital(s), SMA and Aligned Payers. Each of these stakeholders must meet specific requirements and perform certain responsibilities.
The Advisory Council will represent the broader community perspective in shaping the Transformation Plan, and provide continued advisement on Transformation Plan modifications. They will also support hospital and payer recruitment to participate and provide advisory on development of arrangements with payers. While composition of each Advisory Council will be unique, it must include the SMA, at least one participant hospital, at least one aligned payer, and at least one beneficiary or caregiver.
Participant Hospitals have the option to participate with Lead Organizations. They shall be key partners in implementing the Transformation Plan, and must agree to receive a Capitated Payment Amount (CPA) disbursed in bi-weekly payments in lieu of the Participant Hospital’s Medicare FFS payments. The CPA is determined from historical expenditures, and adjusted biannually. They must commit to specific percentages of revenue under CPA in alignment with the Transformation Plan milestones. To be eligible, a Participant Hospital must be an acute care hospital or Critical Access Hospital that meets at least one of the two following criteria:
- Located within the community and receives at least 20% of its eligible Medicare FFS revenue from services provided to residents of the Community, or;
- Independent of facility location, provides services to residents of the community that in aggregate account for at least 20% of the eligible Medicare FFS expenditures of the community
Aligned Payers are critical in supporting financial viability of this model throughout the Community. The goal is to migrate as much revenue as possible under the Advanced Payment Model (APM) to further incentivize transformation. Each Lead Organization must secure multi-payer alignment in the Community. Each Aligned Payer must meet three alignment criteria: financial alignment, operational alignment, and quality alignment.
- Financial alignment: financial methodology that aligns with the selected APM
- Operational alignment: changes to provider contracts or benefits to support care transformation
- Quality alignment: To the extent practicable, use the same set of quality measures to adjust payments and track performance
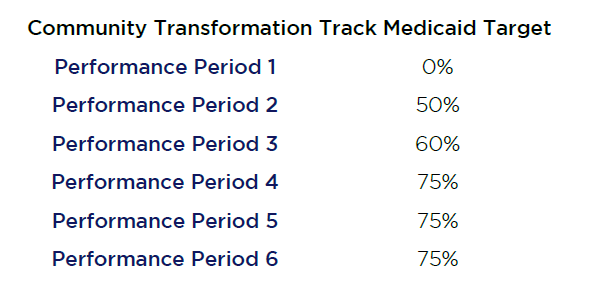
Medicaid participation is required and commercial payer participation is recommended. For Medicaid, the percent of Participant Hospital Medicaid revenue under a CPA arrangement must follow a specific schedule.
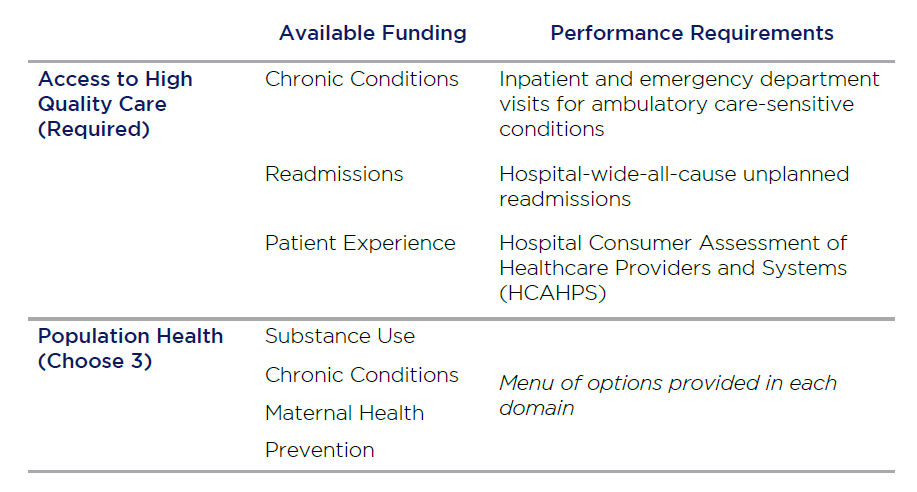
The Community Transformation Track will focus on both Community and Hospital level measures. They include:
Waiver/Benefit Enhancement Opportunities
Medicare waivers allow Participant Hospitals to waive cost sharing for Part B services, provide beneficiaries with transportation, and offer gift card rewards and incentives for chronic disease management programs. Other waivers include:
- Waiver of requirement for a three-day inpatient stay prior to admission to a skilled nursing facility (SNF)
- Telehealth expansion (continued post-Covid-19)
- Post-discharge home visits and care management home visits
- Critical access hospital (CAH) 96-hour rule
- Waiver of Medicare hospital conditions of participation to allow a rural outpatient department and emergency room to be paid as if they were classified as a hospital
Program Timeline
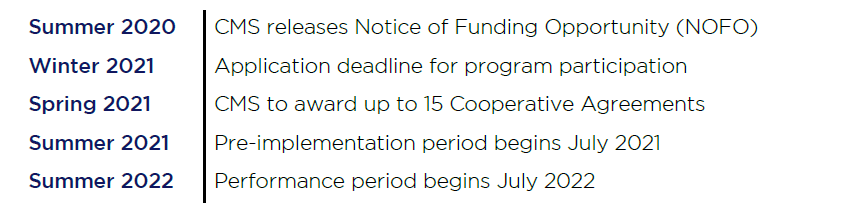
At this time, CMS does not anticipate opening additional application periods.
For more information on the CHART Model Program or the Community Transformation Track contact Shanah Tirado at stirado@copehealthsolutions.com or 213-369-7415.