The One Big Beautiful Bill Act (OBBA) introduces the most significant transformation of Medicaid eligibility since the Affordable Care Act (ACA), placing ACA Expansion Adults at higher risk of coverage loss and exposing large Medi-Cal health plans to $40 to $50 million in annual capitation risk. Beginning December 31, 2026, states must implement six-month redeterminations and monthly work or community engagement verification for individuals covered under the ACA Expansion Adult category.
California has approximately 14.9 million Medi-Cal members. Of these, approximately 5.1 million, or one-third, are ACA Expansion Adults. Under the new requirements, these members will face more frequent renewal cycles, increased documentation expectations, and an elevated risk of procedural termination if plans do not proactively strengthen outreach and support.
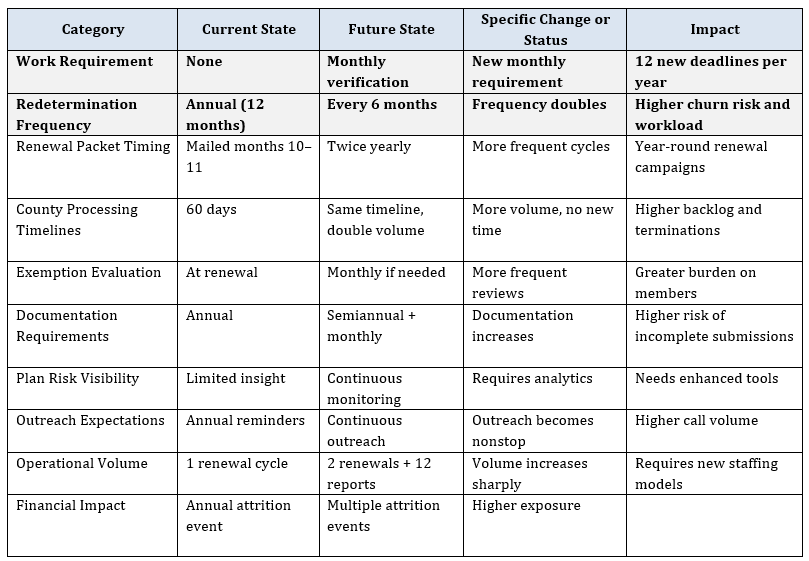
Current eligibility processes already follow strict timelines established by the California Department of Health Care Services. OBBA introduces a second renewal cycle every year for expansion adults and adds monthly reporting expectations, which will significantly increase operational demands on plans, counties, and member support services.
Health plans that begin preparation during 2025/2026 will be positioned to manage the increased complexity, reduce avoidable member churn, protect revenue, improve continuity of care and maintain compliance with state expectations.
Understanding OBBA (H.R. 1) Requirements
Although OBBA creates only two formal requirements for ACA Expansion Adults, the operational impact is far broader. Semi-annual redeterminations and monthly work verification create numerous downstream effects across member outreach, documentation processing, staffing models, county coordination, data integration, and financial performance.
Six Month Redeterminations: Renewal frequency for expansion adults will shift from once annually to once every six months.
Monthly Work or Community Engagement Verification: Expansion adults must verify at least eighty hours per month of qualifying work or community engagement activities unless exempt.
Implementation Timeline:
- December 31, 2025: Federal guidance issued
- December 31, 2026: State implementation deadline
- January 2027: Legislation Effective
Impact on California Medi Cal Plans
Scenario: Large California Medi-Cal Health Plan
Consider a large Medi-Cal health plan operating in California with 600,000 members. Consistent with statewide enrollment patterns, assume one-third (200,000 members) are ACA Expansion Adults. Based on recent DHCS rate certifications, ACA Expansion Adults receive an estimated $350–$450 PMPM, equivalent to $4,200–$5,400 per member per year.
Under this scenario, the financial impact of member disenrollment is modeled as follows:
Attrition Impact Scenarios
1. 5% Attrition Among ACA Expansion Adults
- Members potentially lost: 5% × 200,000 = 10,000 members
- Capitation dollars lost:
- Low estimate: 10,000 × $4,200 = $42 million
- High estimate: 10,000 × $5,400 = $54 million
2. 10% Attrition Among ACA Expansion Adults
- Members potentially lost: 10% × 200,000 = 20,000 members
- Capitation dollars lost:
- Low estimate: 20,000 × $4,200 = $84 million
- High estimate: 20,000 × $5,400 = $108 million
Key Assumptions:
- Total Plan Membership: 600,000
- Share of ACA Expansion Adults: One-third
- ACA Expansion Adults: 200,000
- Capitation Rate Assumption: $350–$450 PMPM
- Annualized PMPY: $4,200–$5,400
Operational Challenges for Medi-Cal Plans
OBBA introduces several operational challenges that require early planning: doubling of renewal volume, monthly work verification, limited visibility into county determinations, and increased DHCS monitoring.
Readiness Framework: Assess, Stratify, Mitigate
- Assess: Evaluate existing workflows, member contact information accuracy, and staffing readiness
- Stratify: Segment members by renewal month, risk level, and reporting vulnerability
- Mitigate: Implement renewal reminders, work requirement education, CHW outreach, and documentation support
How COPE Health Solutions Supports OBBA Readiness
Assess Readiness Across Operations, Data, and Member Support
Evaluate current eligibility workflows, staffing capacity, data infrastructure, and member communication processes to determine preparedness for semi-annual renewals and monthly work verification. Identify gaps and develop a prioritized readiness roadmap to strengthen operational, technical, and member support capabilities. Support with recommendations and integration of technology platforms to streamline recertification workflows through automation and improved member outreach.
Eligibility and Operational Redesign
Redesign workflows that govern renewals, documentation processing, reporting support, and member outreach to align with the continuous cycles required under OBBA. Build operational models that reflect increased volume and ensure predictable, consistent member support.
Data Integration, Analytics, and Reporting
Integrate eligibility, reporting, and outreach data to create unified visibility into renewal and work verification activity. Develop dashboards and monitoring tools that track status, identify risk, and support timely intervention.
County and Provider Coordination
Strengthen communication pathways with counties and providers to streamline information flow and support timely resolution of eligibility or reporting issues. Align all partner touchpoints so members receive consistent guidance and coordinated support.
Workflow Playbooks and Staff Training
Create clear, standardized playbooks that outline roles, workflows, and member support protocols across all teams. Provide targeted training to ensure staff are equipped to manage continuous renewals and monthly verification requirements.
AI Supported Population Management and Risk Identification
Leverage AI to proactively manage OBBA requirements by identifying members at highest risk of procedural disenrollment, forecasting renewal and reporting volume, and detecting early warning signals of coverage disruption. AI enabled workflow automation improves operational efficiency, prioritizes outreach, and streamlines documentation handling to reduce avoidable member attrition.
Top Changes Under OBBA
Call to Action
Medi-Cal plans must begin OBBA readiness planning during 2025. With twice per year redeterminations and monthly verification requirements beginning December 31, 2026, delaying preparation will compress essential work into a narrow window.
Closing
OBBA is a significant transformation in Medi-Cal eligibility and reporting. Plans that prepare early will maintain stability, support vulnerable populations, and reduce unnecessary member churn.
Sources:
Department of Health Care Services
State Health & Value Strategies

