 Current state of health care
Current state of health care
The traditional approach to health care delivery is quickly becoming obsolete as health care shifts from a focus on treatment to prevention. Treating an illness is often far more expensive than providing the preventative care that would deter its onset, and is imperative to developing long-term solutions for population health management. In response, health care providers have developed programs aimed at coordinating patient care. The programs vary widely in structure and style, but all have the goal of improving health outcomes while decreasing overall cost.
There are several limitations to current conventional care coordination programs. Traditionally programs only target specific high-utilizing or high-risk populations, most focusing on patients with specific chronic conditions. For most payors and providers, these investments are into disease management programs: focused care coordination activities or member communications on specific chronic diseases such as diabetes, asthma or congestive heart failure. For most patients, enrollment in these programs results in occasional phone calls assessing patient needs related to a specific chronic illness, health education information via telephonic outreach or mailers, and telephonic follow-up on primary or specialty care visits. Care coordination programs have frequently been found in payor organizations and inpatient settings, with fewer instances of care coordination presence in ambulatory and community health center settings. Although some systems COPE Health Solutions observed were more successful than others in seeing clinical and financial benefits across patient populations, most programs only saw improvement in outcomes for severely ill patients at high risk for hospitalization or re-admission. Lastly, payors and providers have been limited in expanding the investment and scope of these programs due to misaligned incentives or lack of reimbursement for services outside of a conventional fee-for-service fee schedule.
The majority of existing care coordination models fail to acknowledge or address factors outside of the health care system that impact an individual’s overall health status. In other cases, care teams may exist to evaluate external factors; however, these teams often function in silos within the health care setting, with little information on how to engage the resources available such as social workers or community-based organizations. Addressing patient health from a broader perspective includes addressing the social determinants that influence health outcomes, and engaging patients as a collaborative partner in their own wellness. Health systems across the nation are beginning to recognize this dynamic interplay between an individual’s social needs, healthy lifestyles and behaviors, and their corresponding health status. Frequently, health systems cite unmet needs related to behavioral health, substance abuse, housing, access to food, and unemployment as significant contributors to poor outcomes and cost. This holistic approach of patient care has been difficult for health systems to execute on due to the lack of aligned incentives and reimbursement models.
In recent years, payment reform at both federal and state levels have driven health systems to evolve their outlook and investments in care coordination strategies. The passage of the Patient Protection and Affordable Care Act (ACA) in 2010 expanded health insurance access through federal and state-based exchanges, along with the expansion of Medicaid. The increased volume of patients accessing health care has resulted in an increased fiscal burden on states and provider organizations. Sophisticated provider organizations have begun to create and participate in varying Accountable Care Organization (ACOs) models as a way to share financial risk, while incentivizing investments in coordinated, high-quality care. Furthermore, the more recent passage of the Medicare Access and CHIP Reauthorization Act (MACRA) in 2015 has clearly articulated CMS’ roadmap to value-based payment for Medicare within the next five years. This “perfect storm” of market and regulatory reforms has forced health care organizations to expand and execute on strategies that result in improved clinical outcomes while decreasing costs. While the new administration has claimed that much of health reform will be repealed, the ability to “do more with less” is an expectation of all organizations that will persist under the new administration.
In order for payors and providers to remain competitive and financially sustainable in the changing healthcare landscape, organizational strategies must include a comprehensive care coordination component as a key driver to improve clinical outcomes and financial performance. Regardless of type, setting or maturity of a health care organization, core care coordination principles must be adopted to improve patient outcomes and compete in a growing competitive market. This article outline’s COPE Health Solution’s approach to care coordination.
How care coordination can help health systems achieve the Triple Aim
Most stakeholders agree that establishing a care coordination program is key to supporting the Triple Aim: improving the patient experience of care, improving the health of populations and reducing the per capita cost of health1, but there are a variety of ways that organizations define care coordination. The AHRQ defines care coordination as the deliberate organization of all activities related to a patient’s care, including all appropriate providers and other resources needed.[1]
Although this definition is sufficient on a basic level, COPE Health Solutions offers a more comprehensive approach to defining what a robust care coordination program should consider:
- Care coordination exists across the full care continuum. All providers must communicate and work together as a patient moves across settings – including nonclinical providers such as community-based organizations that address social and environmental factors which influence a patient’s ability to thrive.
- Care coordination is enabled by information exchange. The right information technology (IT) infrastructure, integration and exchange is essential to ensure that providers are able to easily, quickly and accurately document and share patient information, including care plans and clinical status changes, to all members of the patient’s care team.
- Care coordination proactively empowers patients and caregivers. Patients and caregivers are given an active role and voice in their care, ensuring their responsibilities are feasible and that the system is easier for them to access and navigate.
Establishing this more robust model is a significant undertaking, particularly in settings where staff feel overburdened and must accommodate care coordination work flows into their scope of work. With the impending transition to value-based payments, developing a strategy and achieving organizational proficiency in care coordination is no longer optional. The heavy initial task of establishing this care coordination infrastructure will pay off by helping providers to achieve the Triple Aim:
- As providers work more closely together and in tandem, they are better able to provide preventive screenings, close gaps in care, ensure patients are seen by the most appropriate provider, and ensure high-risk patients receive timely follow-up appointments.
- By expanding the care continuum beyond the clinical setting, providers can connect patients to resources in the community that will address social determinants of health.
- Patients and caregivers are more likely to adhere to all aspects of the care plan (lifestyle changes, medications, and attending appointments) as the system becomes easier to navigate.
- With better coordination, patients can be directed to the right setting for their health needs, reducing avoidable admissions and ED utilization.
- Appropriate follow-up with high-risk patients can prevent complications and readmissions.
- Connecting patients to primary care providers and monitoring completion of preventive screenings can ultimately prevent the onset of chronic diseases.
- Organizations will begin to proactively identify populations and apply standard protocols to populations, resulting in improved outcomes.
How to put care coordination into action
Whether an organization is just getting started with care coordination, or seeks to move to the next level of proficiency and innovation in care coordination, there are foundational elements of this care approach that must be in place, including:
- An awareness of the patient population. In order to design care coordination programs that meet the Triple Aim, the organization must understand the population it serves. This process of conducting an initial risk stratification, as well as developing an ongoing work flow for re-evaluating and stratifying new patients, is a core competency for any program.
- Patient care programs. Once the population is well understood and segmented, the thoughtful design of programs to support patients can be undertaken. As noted previously, these programs have traditionally taken a disease management stance. In new models of carecoordination, organizations should begin to broaden care coordination efforts to include disease prevention programs alongside disease management programs.
- Patient enrollment and outreach. A consistent, formalized approach to preventing and managing disease has always been the tenet of supporting a patient’s health and wellness. Care coordination programs should establish this approach, by proactively ensuring that they have the means to not only enroll patients in care coordination but to consistently engage with patients at any point across the continuum of care.
- Provider engagement. To successfully execute on care coordination programs, inpatient, primary and specialty providers must be engaged in the programs. Developing the necessary level of engagement means involving the providers in all stages of program development. Engaged providers are well-versed in the composition of their patient populations, the programs available to the patients, how to appropriately document patient care so that care coordination opportunities are flagged by chart review processes or automated systems, and how to encourage or reinforce participation in programs during patient encounters. Achieving this level of engagement may require additional training as well as feedback and support from the care management team.
- Care coordination infrastructure. The foundational elements, as well as additional and advanced capabilities in care coordination, require infrastructure to be successful. Although not all organizations are prepared to make significant IT investments, an electronic medical record that supports discrete data fields and has native reporting capabilities is a necessary baseline system. Such as system will allow the organization to identify patients before migrating them to a manual or third-party system to manage program enrollment and subsequent care management work flows.A more robust infrastructure will consist of a system that provides an analytics platform that supports an end-user defined and applied risk stratification methodology. Additionally, more robust systems will support the end to end care coordination workflow, including alerts and triggers for patient enrollment in programs, task management, reporting at the patient and program level and program “graduation” indicators.
- Work force planning. The final foundational element of a care coordination strategy is the development of a work force. The title “care coordinator” has become more common in the changing healthcare landscape, however each organization must define the appropriate level of licensure to meet the needs of the patient population, as well as create a roadmap to achieve a care coordination team with clear work flows, roles and responsibilities for care coordination.
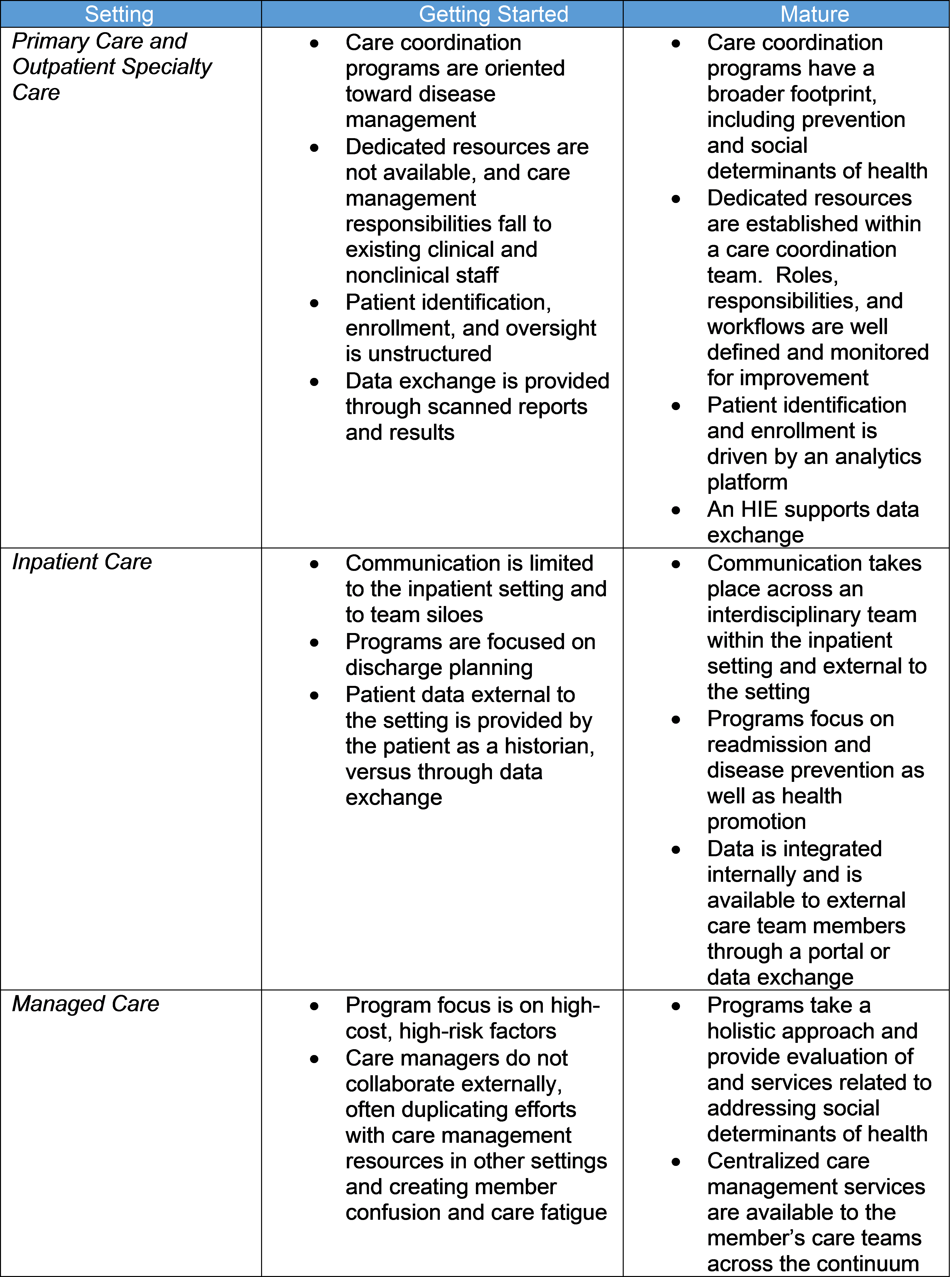
Although the foundational elements of a care coordination program should be the initial focus for any organization, COPE Health Solutions believes that all organizations, regardless of the setting or the current level of competency, can begin to develop a care coordination program and continue to build proficiency. Table 1 below outlines the expectations of specific care settings, ranging from “getting started” to “mature”.
How can COPE Health Solutions help?
COPE Health Solutions partners with health care organizations regardless of where they are in the continuum, to develop customized programs and solutions that address the ever-changing demands of health care systems. In a post-ACA environment, health systems and their respective communities are tasked with providing quality, patient-centered care to diverse populations with even more diverse needs. As health systems increasingly participate in value and risk based contracting, and become more at-risk for meeting specific quality standards, turn-key solutions that encompass strategic planning considerations, workforce gaps and educational needs, and local market trends are imperative in meeting the health care demands of today. COPE Health Solutions can assist your organization with finding the appropriate entry point into care coordination for your organization, or we can work with you to complete a thorough assessment and recommendations on how to get additional value out of your existing program.
1 http://www.ihi.org/engage/initiatives/tripleaim/pages/default.aspx
2 https://www.ahrq.gov/ncepcr/care/coordination/atlas/chapter2.html