 Role of CBOs in VBP
Role of CBOs in VBP
As the healthcare industry shifts towards population health management, integrated delivery systems (IDSs) working with health plans are quickly realizing the need to reimagine traditional partnerships. As incentives drive care out of acute care settings, a focus on preventive care has alerted providers of the need for support outside of traditional clinical settings. More than ever, IDSs are considering the need to address the underlying disparities and social determinants of health to improve outcomes and lower costs.
Community-based organizations (CBOs) are deeply rooted within their communities and provide a wide variety of social and support services to individuals, families, and populations. These services range across housing, job placement, transportation, legal services and mental health services. However, many of these services are traditionally viewed as beyond the scope of healthcare and are often not reimbursed by health plans. These services address unmet needs in the community that impact health and health outcomes but are caused by social and economic factors outside the traditional responsibility of local health systems.
Social determinants of health (SDH) have a significant impact on health outcomes. It is estimated that a third of total deaths in the United States can be attributable to social factors, including economic status, education and discrimination1 New York State (NYS) has identified and evaluated social determinants across five categories where CBOs can potentially engage and provide interventions (see Figure 1 below). To achieve the state’s goal to reduce avoidable hospital readmissions and reach 80-90% value-based payments by 2020, addressing these determinants through population-based approaches will be key.
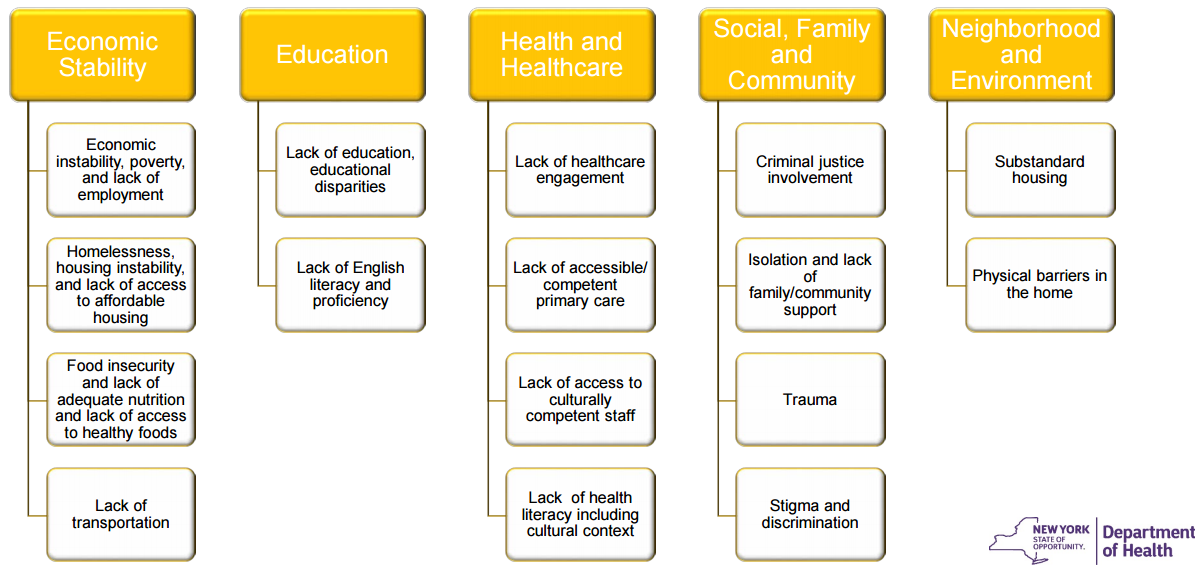
NYS DOH Medicaid Redesign Team, 2015
In addition, the NYS VBP Subcommittee has identified the following categories of CBOs that provide key non-acute community services: 1) health plan billing, clinical services; 2) health plan billing, non-clinical services; and 3) non-billing, community-based human services.
- Billing clinical service providers are licensed by the Department of Health (DOH), Office of Mental Health (OHM), or the Office of Alcoholism and Substance Abuse (OASAS). These organizations provide clinical support and care management services in acute and post-acute care settings. CBOs within this category can play a role in reinforcing primary care and supporting transitions between care levels. Services such as chronic disease management, medication management, and care transitions are widely accepted as effective interventions to reduce hospital readmissions and associated costs.
- Billing, non-clinical service providers support the physical needs of patients in the post-acute to home setting. CBOs within this category support patients and help them thrive in lower levels of care by providing services such as transportation, home and family assessments, and caregiver support.
- Non-billing, community-based human service organizations assist patients with everyday assistance in the home and social setting for services not covered by health plans. These organizations provide services such as housing, nutrition, job placement and judicial assistance.
In a report to Congress in 20132, the Centers for Medicare & Medicaid Services (CMS) described a retrospective evaluation of the effectiveness of community-based wellness and prevention programs. The published literature examined in CMS’s evidence review and in its initial evaluations of potential program effects indicate that these programs have the potential to improve health outcomes and reduce healthcare costs for beneficiaries. Specifically, several chronic disease self-management and physical activity programs offered by CBOs demonstrated reductions in costs related to unplanned hospital visits and have shown lower total healthcare costs for participating beneficiaries. Moving forward with VBP, providers and provider networks have an opportunity to fill critical gaps in care through partnerships with CBOs. By combining capabilities across the three categories, provider systems can bolster efforts to establish cost-effective care that is coordinated around members.
Road to Integration
Despite general understanding that CBOs, both billing and non-billing, are important actors in improving health outcomes through social determinants of health, it is less understood what the ultimate impact on costs and utilization might be. To date there have only been a handful of studies that have directly addressed the impact of CBO services on cost and utilization outcomes. The few studies that address these issues have not had sufficient power to identify statistically significant effects. This lack of information may prove to be a significant barrier to more widespread dissemination and implementation of these interventions by formal health systems or payors. As CBOs across all categories, continue to develop and strengthen their relationships with health systems, they will need to measure, quantify and communicate their value-add.
Issues such as capacity constraints, volunteer staffing, small budgets, precarious finances and unsophisticated management are all aspects of many CBOs and will pose significant challenges. Additionally, addressing SDH at both the member and community level may not result in immediate savings on what are often aggressive VBP timelines. This will require the design and implementation of innovative payment mechanisms to incentivize and reward SDH interventions in VBP arrangements when the services provided are less tangible. Many CBO programs currently depend on limited grant dollars from various federal funding streams; without innovative direct payment mechanisms, the reach of their interventions may be limited.
CBOs will have to expand their business acumen to negotiate with healthcare entities. This will entail developing a variety of internal organizational capabilities before they are able to enter into mutually beneficial partnerships with the health systems. In this new environment, CBOs may indeed make a convincing business case that their services create value for their potential clients and partners (hospitals, post-acute care providers, provider networks and insurers). However, heavy reliance on CBOs as a routine reliable aspect on the healthcare continuum has not been tested on the large scale that the healthcare industry and government payors require of dependable partners. Core competencies such as analytical competencies to measure and quantify the impact of their organization, marketing strategy to communicate their value, and competitive analysis will be key to successful differentiation and integration into VBP contracts.
DSRIP as a Means to Integration
In New York State, CBOs have an opportunity to utilize the Delivery System Reform Incentive Program (DSRIP), a proponent of the 1115 Waiver, to enter into VBP arrangements with provider networks. DSRIP has been a driving force behind the adoption of VBP in the state, aiming to promote collaboration, reduce avoidable hospital use by 25% over five years and financially stabilize the state’s safety net through payment reform. Performing Provider Systems (PPS) in New York State’s DSRIP program are tasked with the development of IDSs and are expected to tie care delivery transformation to VBP within their service areas.
In July 2015, CMS approved the New York State Roadmap for Medicaid Payment Reform to ensure the long-term sustainability of the improvements made possible by DSRIP. The multi-year roadmap details the State’s vision for comprehensive Medicaid payment reform, including how the state will amend its contracts with MCOs. New York State has committed to reaching 80-90% VBP by 2020, which will require new approaches for reimbursement and partnerships between MCOs and providers that align with DSRIP objectives. As care is shifted away from inpatient settings and into communities, partnerships between CBOs and PPSs will become increasingly valuable.
The NYS DOH Office of Health Insurance Programs recently issued a request for applications to announce the availability of funds for the support of CBOs in specific targeted areas that remain un-served/underserved as part of the DSRIP Program3. These funds will be distributed as grants to assist CBOs in planning activities to identify business requirements and formulate strategies for short-term needs as well as longer term plans that the CBO may envision in system transformation. This will allow organizations to better position themselves for continuing engagement with PPSs in DSRIP projects, and consequently, value-based payment and contracting. Grant programs, such as this, offer CBOs an opportunity to build sustainable pathways towards value-based payment arrangements. Immediate strategies to focus on may include: implementation of electronic health records capable of capturing patient populations and participating in bidirectional exchange; developing and improving core business processes; and funding studies to build an evidence-base for addressing social determinants of health and quantifying impact on costs.
Moving Forward
Healthcare payment reform and delivery system integration has created a unique opportunity to reimagine how care is delivered outside the four walls of hospitals and physician offices. With increased attention on improving population health, the relationships that delivery systems foster with their community resources will be key to successful reform. As these relationships mature, VBP contractors can build upon their knowledge of critical success factors to improve outcomes and demonstrate return on investment.
About COPE Health Solutions
COPE Health Solutions is a national health care consulting that advises hospitals and health care systems on strategy, population health management, Medicaid waivers and workforce development solutions. COPE Health Solutions provides clients with the tools, services and advice they need to be leaders in the health care industry. COPE Health Solutions is currently working with multiple participants of the New York State DSRIP program to align their performance-based contracting methodologies with desired future goals of VBP readiness. Contact DSRIP@copehealthsolutions.com to learn more.
Footnotes:
1 Galea, Sandro et al.. “Estimated Deaths Attributable to Social Factors in the United States. “American Journal of Public Health 101.8 (2011): 1456-465. Web.
2 https://innovation.cms.gov/Files/reports/CommunityWellnessRTC.pdf
3 https://www.health.ny.gov/funding/rfa/1512160408/index.htm
