Background
A risk bearing entity’s (RBE) ability to bear financial risk profitably is based on its ability to consistently manage the utilization and health outcomes of its attributed population. In today’s market, to be a RBE is to be in the business of care management. Successful care management is a critical competency that organizations must either build or buy in order to remain economically sustainable in a value-based payment (VBP) environment. CMS, self-insured employers and some states have made it clear that providers are expected to be able to take risk in order to ensure financial incentives for total cost of care and quality are aligned.
Care management, like most aspects of the health care business, is not one-size-fits-all. While the market is beginning to converge on what to do, there is still the hurdle of figuring out how to do it within your organization and a broader network of providers. Understanding what to do for specific transitions of care, high risk attributed or assigned members, populations or service lines is essential knowledge and builds a cohesive care management strategy that supports a suite of initiatives that is more complex. Scale, interoperability and cross-functional alignment are critical success factors in managing total cost of care. To be impactful in population health and on the bottom line, care management must also be well integrated with contracting, finance and network development. In this first of a three-part series exploring the fundamental organization, financial and operational alignment functions of care management, we examine various care management models and how they can be governed and integrated into an organization or network.
There are three general models of establishing organizational care management for a RBE; Decentralized, Federated and Centralized models.
In a decentralized model, the RBE gives a large degree of operational autonomy to subcontracted providers. These providers, often operating under a percent of premium, are held often to performance and outcomes-based standards, but how they get there can be highly varied between subcontracted providers. Financial incentive and sub-contract design is the primary lever of managing the network. Integrating across subcontracted entities is not under the direct control of the RBE.
A federated model sits in the middle of this continuum and is the most common solution in transitioning silos under fee -or-service (FFS) models toward coordinated, high performing networks. While leveraging delegation to navigate business and market realities, there is a deliberate effort to design a cohesive overarching governance structure to pull the various stakeholders together under a collective with clear lines of accountability and authority. Financial incentives are designed to support this structure and the work is in creating mutual value for all parties. This model organizes efforts and aligns operations across centralized and delegated stakeholders that care for the same population, often but not exclusively defined regionally.
In a centralized model, the majority of downstream providers are employed or contracted under collective arrangements. Care management decision-making and infrastructure are centralized and standardized across providers. Both operations and governance align finances, incentives, and activities under a single umbrella. It is important to note that in most cases there are centralized components of care management, while other components are deliberatedly decentralized. These decisions, however, are consistent across the network.
Figure A: Financial, Operational, and Organizational/Governance Influence by Model
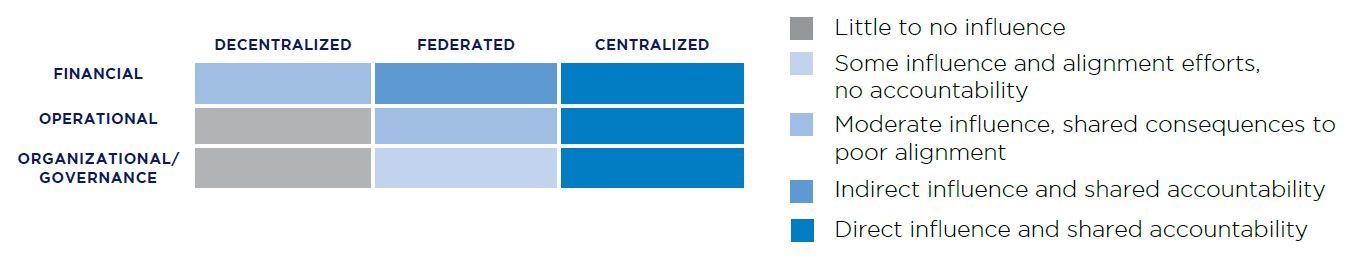
In all models, organizational alignment is foundational to success. Clear channels of communication, data exchange, and a common set of goals and boundaries are the minimum to ensure the members managed under any structure experience well-coordinated and effectively managed care.
Driving Organizational Alignment
Many RBEs seeking to establish care management programs attempt to build on a service-line-by-service-line or condition-by-condition basis. This can lead to narrow definitions of the scope of care management teams and staffing plans designed to meet the envisioned scope within a single, siloed unit or initiative. This often results in redundant programs and challenges in patient engagement/adherence. The corollary pitfall is the development of reactive IT solutions to meet individual documentation and reporting needs necessitating multiple workflows versus a streamlined IT approach. Part of the challenge in establishing more holistic approaches is the absence of organizational channels to make the decisions and funnel the resources in a coordinated manner.
The most successful RBEs focus on the whole person and therefore develop care management models that can address multiple co-morbidities while also integrating evidence-based disease management programs for common conditions, such as diabetes. These RBEs often marry high-risk clinics with their care management program, identifying the highest risk, or highest potential risk attributed members and engaging them with a highly trained team who can work with the member to stabilize their condition in collaboration with the PCP.
Governance
In developing an effective care management function, independent of the model chosen, accountability and authority runs through a clear reporting structure to a central care management organization. This requires thoughtful inclusion of network members on boards, committees and workgroups to develop and implement care models, evaluate network and provider performance and correct course of action. Typically, these bodies are organized into finance and administration, clinical care delivery, and network management and provider relations. While the design of an ideal governance structure can be challenging, implementing requires trust building, addressing unspoken and long neglected challenges, and establishing an often uncomfortable level of transparency to lay the groundwork for value creation and collaboration.
Figure B. Sample Centralized Care Management Organization Governance Structure
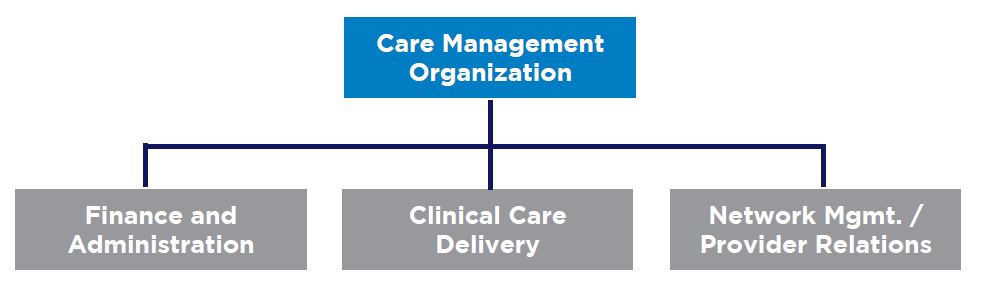
Cross-Functional Integration
These committees and workgroups create the forum for close collaboration between clinical best practice and internal finance and managed care contracting functions to bring alignment to the structure of payor and MCO incentives down through the prioritization of populations and clinical interventions through downstream contracting. It transforms the role of utilization management from a barrier to a partner in care management. Lastly, it aligns organizational budgeting and resource allocation efforts with the work that needs to be done. This feedback loop empowers providers to shape the financial incentives and performance measure targets in a manner where they feel set up for success. Analogously, finance and contracting functions can negotiate with confidence and transparency in the network’s ability to deliver. While a fully integrated and centralized model is difficult to establish, many features of that model can be embedded into the organization to drive strategic and financial rigor and prepare the network for more advanced VBP models.
Inter-Organizational Integration
More sophisticated and robust approaches to care management embed the care management function throughout the RBE and its contracted network providers, identifying and targeting care management transactions that take place across a broad array of settings and establishing roles and responsibilities to ensure the attributed or assigned member’s needs are met regardless of where the transition in care takes place.
In these more comprehensive models of care, leadership establishes key relationships formally and defines roles and standard processes clearly to drive care management success. Leaders then develop success metrics and implement integrated technology essential to successful care transitions and management. The RBE and its contracted providers proactively identify attributed or assigned member needs and trigger pre-defined processes, limiting reactivity and improving the efficiency and quality of care delivery. Importantly, this needs to be inclusive of social service providers not traditionally embedded into core workflows, network development efforts, contracting models and billing infrastructure. A robust care management strategy integrates clinical and social determinants of health (SDOH) into all aspects of the model.
Organizational Alignment as a Vehicle for Financial and Operational Alignment
While organizational alignment creates the internal infrastructure through which to operate a care management program, the design and deployment of these aligned resources is where the rubber meets the road. The alignment of financial incentives empowers all parties involved to sustainably engage in best practice care management; aligned processes and operations coordinate the functions and care delivery so that ultimately the patient reaps the benefits.
Look out for parts two and three, where we dive deeper into driving financial alignment and operational alignment in organizational care management.

