This is part one of a series of articles focused on FQHCs and FQHC Look-Alikes. These community health centers can play a critical role in managing population health and achieving success in value-based contracts.
Many communities struggle with access to high quality primary care services for their residents with lower incomes. Language and cultural barriers combine with financial and transportation difficulties to block health care delivery in medically underserved areas. Neighborhood primary care clinics fill the health care gaps in many localities, delivering culturally-appropriate care on a no or low-cost basis. Federal health policy in 1989, modernized and funded the work of these clinics, formalizing many of these neighborhood clinics into Federally Qualified Health Centers (FQHCs) and a more restricted classification of FQHC “Look-Alike”1.
FQHCs and FQHC Look-Alikes receive enhanced reimbursement through a cost based Prospective Payment System (PPS)2. The lure of better economics, expanded services and access to ambulatory care has led many community health advocates and providers to encourage more FQHCs and FQHC Look-Alikes.
The FQHC and FQHC Look-Alike programs overcome geographic, cultural, linguistic and other barriers that persist in today’s health care access environment. Because of their close community integration, FQHCs, along with community based organizations (CBOs), play a critical role in successful population health management by addressing the enormous impact of social determinants of health (SDOH).
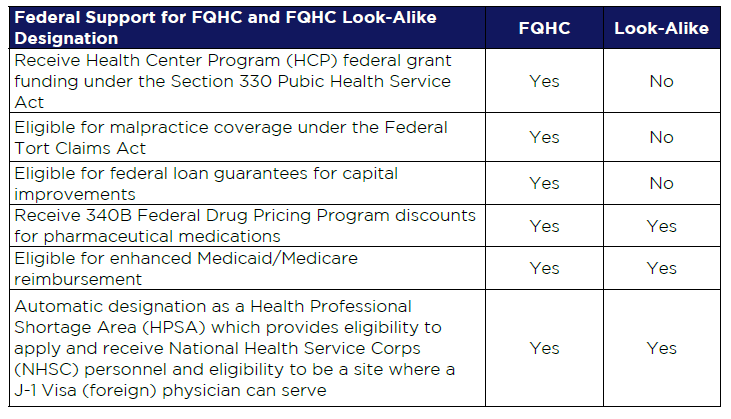
Table 1: FQHC vs FQHC Look-Alike
Designation Key differences and similarities between FQHCs and FQHC Look-Alikes
Becoming an FQHC or FQHC Look-Alike
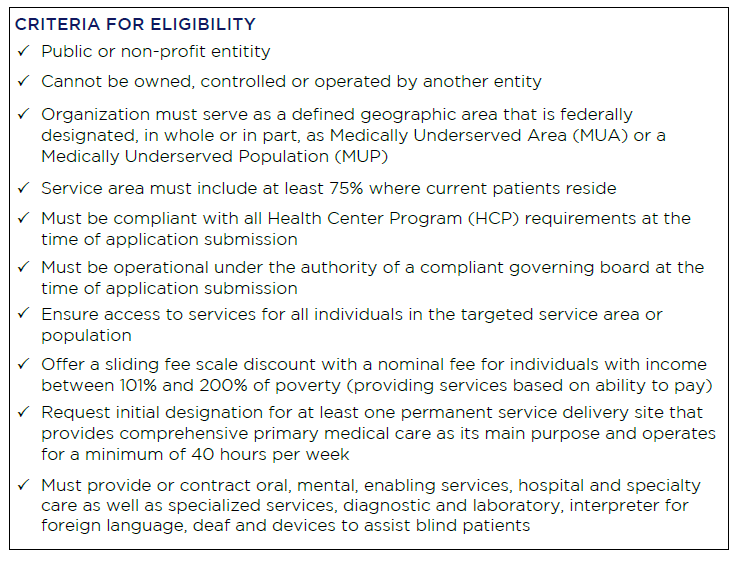
As communities weigh the promise and practicalities of an FQHC or FQHC Look-Alike, many strategic and practical evaluations ensue. There are a number of requirements these organizations need to meet, as outlined by the Health Resources and Services Administration (HRSA). The table below provides a high level summary of these requirements, which include public or nonprofit status, serving patients in an area designated as a medically underserved area or medically underserved population, and the requirement to serve all patients – regardless of their ability to pay.
FQHC Value Propositions to the Community
FQHCs and FQHC Look-Alikes are great partners for health systems, independent practice associations (IPAs) and others based on the following value propositions:
- Aligned missions in better serving the community
- Enhanced Medicaid and Medicare reimbursement
- Increased access
- Eligible for quality incentive dollars based quality indicators
- Increased enabling services (e.g., interpretation, transportation, care management, health education)
- Sliding fee scale providing services to patients no matter their ability to pay
The health centers receive enhanced FQHC reimbursement based on actual costs. This differs greatly from clinics that are paid according to externally established and negotiated fee schedules. Further, FQHCs have access to 340B drug pricing program.
For hospitals and health systems, an FQHC partner in community care offers opportunities to reduce avoidable emergency department (ED) admissions and better coordinate care for the most vulnerable patients. IPAs and health systems can work in collaboration with the FQHC to help fund case managers/care managers and better manage high utilizers of the ED.
IPAs can also fund specialty care in the FQHC sites to leverage the enhanced reimbursement and reduce the specialty cost the IPA is experiencing. Further, IPAs can provide their contracted providers improved bargaining power to negotiate contracts with health plans.
Additionally, providers do not always have the means to provide comprehensive care such as the enabling resources that are needed to address the SDOH. FQHCs can help fill these gaps by providing high quality, integrated primary care with these enabling services, such as care management, transportation and interpretation, to treat the full person.
For example, Adventist Health White Memorial’s service area in East Los Angeles has a higher proportion of unemployed residents and a higher percentage of residents living below the federal poverty level (FPL). It was essential to determine the most viable and sustainable strategy to incorporate an FQHC model in coordination with the overall ambulatory care strategy for Medicaid patients. Their goals:
- Co-location to enhance the clinical integration strategy to enable a more sustainable all-payor health system
- Provide an additional option for physician alignment
- Strengthen the referral network for post-inpatient discharge and ED patients in need of follow-up care
- Integrate Adventist Health White Memorial’s teaching programs
- Improve access to specialty care in a medically underserved community
- Provide high need dental and behavioral health services
Stay tuned for the next article in this series titled “Critical Success Factors in Becoming an FQHC or FQHC Look-Alike.”
For more information, please contact Sarin Khachatourians, Senior Consultant, at skhachatourians@copehealthsolutions.com or 213-598-9331 or Kathy Walker, Executive Consultant, at kwalker@copehealthsolutions.com or 530-713-0214.
Endnotes
1 A ‘Look-Alike’ is an organization that meets all of the eligibility requirements of an organization that receives a PHS Section 330 grant, but does not receive grant funding. Look-Alikes receive many of the same benefits as FQHCs, such as eligibility to purchase prescription and non-prescription medications for outpatients at reduced cost through the 340B Drug Pricing Program.
2 Reimbursement under the Prospective Payment System (PPS), in which Medicare payment is made based on a national rate which is adjusted based on the location of where the services are furnished. The rate increases by 34.16 percent when a patient is new to the FQHC/Look-Alike, or an Initial Preventive Physical Exam (IPPE) or Annual Wellness Visit (AWV) is furnished. Reduced cost drug access from the 340(b) program is offered. The HPSA designation further provides eligibility to apply to receive National Health Service Corps (NHSC) personnel and eligibility to be a site where a J-1 Visa physician can serve.
