 As healthcare delivery in the US matures from a fee-for-service payment model to one that incentivizes quality and outcomes through value-based-payments, coordinated redesign of clinical processes is foundational on the pathway towards transformation. Siloed care delivery must become a vestige of the past, and highly-integrated, patient-centric care must become the new focus in order to achieve all three dimensions of the Institute for Healthcare Improvement’s Triple Aim1:
As healthcare delivery in the US matures from a fee-for-service payment model to one that incentivizes quality and outcomes through value-based-payments, coordinated redesign of clinical processes is foundational on the pathway towards transformation. Siloed care delivery must become a vestige of the past, and highly-integrated, patient-centric care must become the new focus in order to achieve all three dimensions of the Institute for Healthcare Improvement’s Triple Aim1:
- Improved patient experience
- Improved health of populations
- Reduced per capita cost of healthcare
In an attempt to jumpstart clinical redesign initiatives, a number of states have instituted delivery redesign incentive programs that nudge healthcare providers in the right direction, both through facilitating the design of integrated care workflows and through providing incentive funds to enable transformation.
Context for transformation
The Delivery System Reform Incentive Payment (DSRIP) program is a payment and care transformation model various states have implemented in the past decade to transform the way services are provided to Medicaid beneficiaries. While DSRIP takes on many shapes and objectives across the nation, the intent at large focuses on increasing the value of the Medicaid dollar through clinical transformation and care redesign. The New York State Department of Health (NYSDOH) has taken this initiative a step further, and is leveraging DSRIP to address long-term financial transformation, as demonstrated by the recently released final draft of its Value-based Payment Roadmap for public comment2.
Through DSRIP, hospitals, health systems, community providers and community-based organizations are organized into Performing Provider Systems (PPSs), and are responsible for selecting clinical redesign “projects” that incentivize integrated care across the continuum of care. The goal of these projects is to improve access and outcomes, while systematically reorganizing care delivery to root out avoidable utilization and system waste – ultimately increasing tangible value to the payers and consumers.
Transforming care from 2-D to 3-D
In order to drive implementation, the waiver links projects to incentive payments that will be paid upon appropriate completion and documentation of metrics. These metrics are designed to encourage a PPS to operate in a more integrated manner. Yet, although these projects are intended to drive transformation of the delivery system, the program lacks a coordinated strategy to truly connect the dots between individual projects. This can result in siloed projects that, albeit effective during DSRIP, will likely fail to materialize into a sustainable integrated delivery system in the years post-DSRIP. To safely navigate these waters, there is a need for a holistic and cross-functional understanding of DSRIP on all levels, from “2-D” projects to “3-D” integrated healthcare systems. Process mapping is a strategy to bridge this gap.
How, then, does a PPS transition from a flat project design to a 3-D synergistic system? The answer lies in COPE Health Solutions’ clinical redesign expertise. Through a profound understanding of DSRIP, COPE Health Solutions is able to build vertical relationships from specific processes.
Take, for example, a process in which a patient is discharged from the hospital. From a hospital provider perspective, this could be viewed as the end of a care pathway (project) — a patient’s acute care need was stabilized and he can leave. However, from the perspective of an integrated delivery system, it matters what care the patient receives after discharge in order to successfully manage conditions and/or prevent readmissions. This will become especially pertinent as health systems begin to take global risk for the whole care continuum and need to manage utilization.
How process mapping can achieve success
Process mapping is a common technique utilized in project design and process improvement. Its function is to capture the inputs and outputs, parties involved and interactions through the flow of a process. In the context of a DSRIP project, process maps serve as a high-level overview of patient flow through and across the continuum of care, providing the foundation to define partner roles and value (impact on outcomes) in the care pathway.
Figure 1. Simplified DSRIP Project Process Map
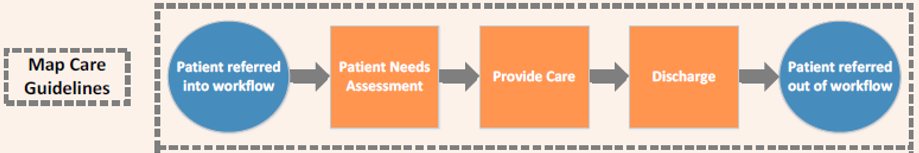
Process maps provide a means to capture the healthcare provider types and their interactions as they follow a patient through their care from start (i.e. a referral) to end (i.e. acute care need stabilized) of a specific clinical pathway. Such diagrams provide an effective tool to map care guidelines for a specific project, but alone still fall short of connecting the dots across the continuum as part of a value-based, coordinated model of care.
To expand, nearly every single process step becomes a foundation for verticals to grow upon. These verticals identify gaps in care which are historically a common source of poor outcomes. The process is iterative, and with each review of the map, one must ask questions that uncover unmet care needs, such as:
- Should the patient receive ongoing or short-term home-care?
- Should the patient be assigned a care navigator to perform outreach and follow-up?
- If the patient was prescribed medication, how can we ensure their adherence?
- Were behavioral health needs identified?
- Was the patient’s visit documented in an EMR? If so, can future providers view it?
Figure 2. Verticals Built onto Process Map Steps

By approaching process mapping, and ultimately project design, in this way, these gaps in care identified by the verticals become more apparent and facilitate the coordination of providers, but also the DSRIP projects as a whole. What is constructed is a series of verticals that, when connected, create a full care continuum and value stream. Each vertical leads to another care workflow that a patient can be routed into as needs are identified:
Figure 3. Care Workflow Network Built from Verticals
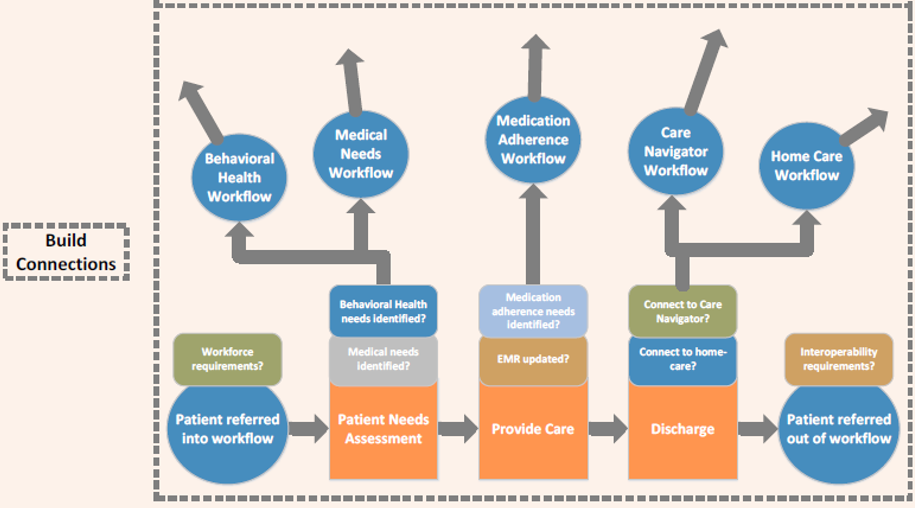
The result is a “spider-web” care network of integrated DSRIP projects, consisting of processes which are intentionally designed to address patient care needs throughout the continuum of care. The care delivery network experience, therefore, becomes seamless, with interconnected DSRIP projects acting as the care guideline threads on which patients move. These threads that assess patient needs in the population enable providers to visualize and balance appropriate degrees of risk with proper levels of care.
Enhanced process mapping of DSRIP projects is an effective means to identify and plan the path to clinical redesign. Visualizing care workflows and the overlaps between them informs many aspects of project implementation. At a high level, it may be lead to the identification of interoperability needs that require IT investment, or to the prioritization of workflows that necessitate a workforce investment. Furthermore, on a more granular level that focuses on the health system network of providers, process mapping leads to better partner selection criteria, and refined responsibilities of each partner in a workflow, thus informing partner relationships and network development.
By capturing processes in this way, the health care system is able to boost the value of the Medicaid dollar, navigate patients longitudinally through the continuum of care, all whilst constructing an IDS capable of population health and patient-centric care.
About COPE Health Solutions
COPE Health Solutions is a health care consulting firm that advises hospitals and health care systems on strategy, population health management, Medicaid waivers and workforce development solutions. COPE Health Solutions provides clients with the tools, services and advice they need to be leaders in the health care industry.
For more information, please contact info@copehealthsolutions.com.
[1] Institute for Healthcare Improvement, IHI Triple Aim Initiative (2016)
[2] New York State Department of Health, A Path Toward Value Based Payment: Annual Update (March 2016)
