 Nationally, the drive to improve health outcomes, enhance patient/member satisfaction and reduce total annual cost per member is requiring both providers and health plans to re-evaluate their contracts and the structure of their financial relationships. The health care industry and its payers, both government and commercial, are rapidly shifting from fee-for-service to a value-based payment model in an effort to achieve the goals of improved quality, enhanced member experience and reduced global per member cost. Success in this new environment requires significant care coordination infrastructure and supports that the majority of small independent physician groups, solo practitioners and other stand-alone providers may find too expensive to implement and sustain without some sort of scale and support structure. Many do not have the size to negotiate favorable contracts with health plans, the resources to invest in all of the systems needed to remain cutting edge like electronic health records, or the market share to compete with both hospital-employed physician groups and large independent practice associations (IPAs).
Nationally, the drive to improve health outcomes, enhance patient/member satisfaction and reduce total annual cost per member is requiring both providers and health plans to re-evaluate their contracts and the structure of their financial relationships. The health care industry and its payers, both government and commercial, are rapidly shifting from fee-for-service to a value-based payment model in an effort to achieve the goals of improved quality, enhanced member experience and reduced global per member cost. Success in this new environment requires significant care coordination infrastructure and supports that the majority of small independent physician groups, solo practitioners and other stand-alone providers may find too expensive to implement and sustain without some sort of scale and support structure. Many do not have the size to negotiate favorable contracts with health plans, the resources to invest in all of the systems needed to remain cutting edge like electronic health records, or the market share to compete with both hospital-employed physician groups and large independent practice associations (IPAs).
The number of solo physicians and small independent group practices is declining and will continue to decline. In 2014, only 17% of physicians remained in solo practice, down from 25% in 2012. Similarly, only 35% of physicians were independent practice owners, down from 49% in 2012 according to a September 2014 survey by The Physicians Foundation and Merritt Hawkins.
 While some physicians are heading into retirement or seeking hospital employment opportunities, others are turning to IPAs as their new business model. IPAs enable physicians to retain their independence, while helping them create the kind of synergy needed around a common set of patients to provide better and more cost effective care. Physicians—especially small independent group practices—can’t reorganize care delivery unless they can grab capitated dollars to align financial incentives and fund this type of care transformation in a sustainable manner. If physicians want to drive care and be health care leaders, they need to be part of an IPA or have some sort of risk agreement that enables them to benefit from reducing hospital admissions and doctor visits. IPAs can not only help physicians manage the patient population and the continuum of care, but can also pass risk and dollars from health plans to providers so everyone can share in the financial benefits and risks of decreasing admissions.
While some physicians are heading into retirement or seeking hospital employment opportunities, others are turning to IPAs as their new business model. IPAs enable physicians to retain their independence, while helping them create the kind of synergy needed around a common set of patients to provide better and more cost effective care. Physicians—especially small independent group practices—can’t reorganize care delivery unless they can grab capitated dollars to align financial incentives and fund this type of care transformation in a sustainable manner. If physicians want to drive care and be health care leaders, they need to be part of an IPA or have some sort of risk agreement that enables them to benefit from reducing hospital admissions and doctor visits. IPAs can not only help physicians manage the patient population and the continuum of care, but can also pass risk and dollars from health plans to providers so everyone can share in the financial benefits and risks of decreasing admissions.
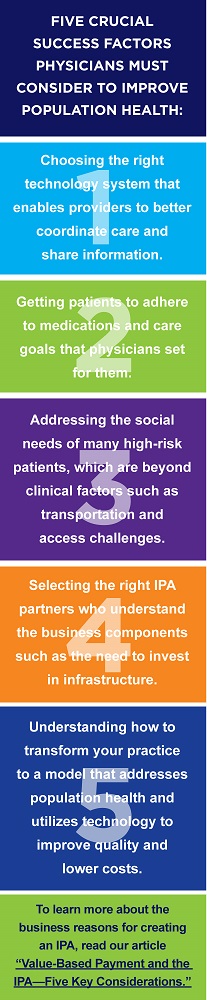
When developing an IPA as part of a broader population health strategy, providers should focus on the following three key elements:
- Determine your target population. Providers should determine who their target population is and based on that population evaluate their needs. What types of providers do they need in their network beyond the traditional primary and specialty care physicians? Providers should be partnering with behavioral health specialists, long-term care facilities and home health agencies, for example. By incorporating behavioral health clinicians into primary care settings, providers can truly begin to change how health care is delivered to at-risk patient populations. This type of integration makes it easier for physicians to provide high quality care to patients and makes it easier for patients to access the care they need.
- Develop economies of scale. As providers come together in an IPA model, they are better equipped to negotiate rates with health plans and engage with hospitals as referral partners for admissions. For physicians to succeed under health care reform, they need to have shared systems, common care delivery guidelines, and a strong infrastructure to manage patient experience and the continuum of care. In terms of tools and resources, it is important to have the ability to provide real-time data at the point of care for physicians. Providers need a strong web-based platform equipped to pull claims data from health plans, as well as patient care data from other providers in the network. It needs to be a strong platform with multiple inputs that is not cumbersome for physicians to use. Ideally, the platform is a single sign-on model with proactive communication tools, so physicians can receive alerts about patient admissions, discharges, and transfers.Physicians should also receive clinical reminders for patients, such as diagnostics and recommended screenings, and have the ability to view patients in various ways either by age or disease state or risk. For example, if physicians can see which patients are high-risk and overdue for care and the IPA has a strong outreach arm (including patient care extenders and patient care navigators to bring patients in for needed follow up care), then the IPA can improve outcomes, reduce costs, and increase value. It is critical to have a care model that places patients into buckets of risk—high, medium, and low—so providers can focus on high-risk and high-cost patients.
- Build a strong brand. Providers should look for ways to gain recognition as a leader in the market in order to increase penetration in the market. They should position themselves to better manage the continuum of care for their patients which, ultimately, will improve their financial bottom line as well as the outcomes of their patient population. One element of building a better brand is hiring the right medical director for the IPA. It should be someone experienced in both inpatient care, specialty care and, ideally, with a prior role in utilization management and quality improvement. It is also helpful to have a practicing physician—someone who understands the current challenges and opportunities in the health care industry. The medical director may be the most critical person in the IPA, because they can ensure that physicians adhere to the clinical guidelines and standards of care required to meet the needs of health plans, patients, and other providers in the network in order to control costs and improve quality.
For more information and for help developing, assessing, implementing or managing an IPA, please contact: consulting@copehealthsolutions.com.

