On October 3rd, 2023, CMS published an ACO REACH Newsletter providing PY23 HEDR submission procedure and timeframe updates.
Health Equity advancement is a fundamental component of the ACO REACH model and a key differentiator from its predecessor, the Global and Professional Direct Contracting Model (GPDC). CMS established HEDR requirements for REACH ACOs as part of the model’s efforts to achieve health equity. To meet HEDR requirements, REACH ACOs must submit beneficiary-level demographic and social determinants of health (SDoH) data representing all aligned beneficiaries to CMS. PY23 HEDR data submission procedures and timeframes have been unclear, however, after CMS announced multiple updates to them since the beginning of PY23.
Here are 5 things to know about HEDR submissions:
1. REACH ACOs are financially accountable for submitting HEDR data. CMS applies an HEDR adjustment to a REACH ACO’s Total Quality Score, based on the formula below.
Total Quality Score = [Initial Quality Score * Continuous Improvement/Sustained Exceptional Performance (CI/SEP) Multiplier] + HEDR Adjustment
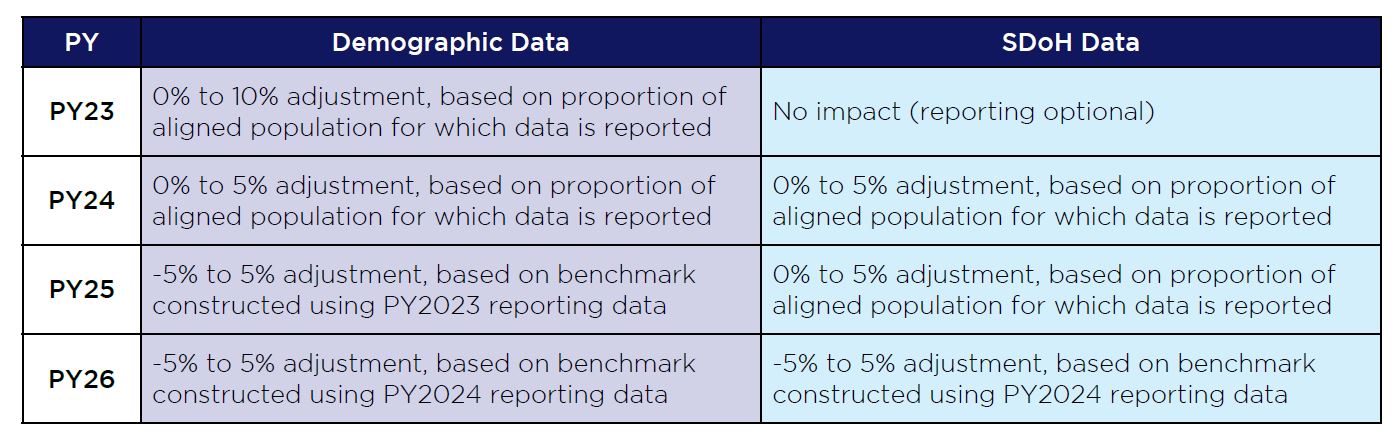
The Total Quality Score then governs the amount of the 2% quality withhold applied to the PY benchmark that REACH ACOs will earn back at the Financial Settlement. Out of the 100 percentage points available for the Total Quality Score, the HEDR adjustment contributes up to 10 percentage points across plan years, as illustrated in the table below.
The remaining percentage points are determined by the REACH ACO’s performance against performance measures across plan years.
2. HEDR demographic and SDoH data components required for submission will expand after PY23. In PY23, only select demographic data will be required for submission, specifically beneficiary name, MBI, sex assigned at birth, race, ethnicity, preferred language. CMS will not require SDoH data for submission in PY23. In PY24 and beyond, however, CMS will require three additional demographic data elements, namely expanded ethnicity categories, sexual orientation and gender identity, and all SDoH data elements for submission. SDoH data largely includes responses to CMS-selected questions from one of three SDoH screening tools: the CMS American Health Communities (AHC) Health-Related Social Needs (HRSN) Screening Tool, the North Carolina Department of Health and Human Services (NCDHHS) Medicaid SDoH Screening Questions or the NACHC PRAPARE Screening Tool. CHS advises REACH ACOs to carefully examine its currently available data to ensure it aligns with CMS pre-populated response options and there is a clear path to capturing outstanding data. For many demographic data fields, for example, REACH ACOs are permitted to submit “Choose Not to Disclose” or “Asked But Unknown” for data fields that beneficiaries are unwilling to answer, such as Race or Ethnicity. CMS does not apply this flexibility, however, to the demographic data field “Languages Spoken”. For this, REACH ACOs must receive a response from beneficiaries that align with one of the 183 available options. If an inadmissible response for “Languages Spoken”, such as Yugoslavian, is currently listed on a provider’s EMR on the behalf of an aligned beneficiary, CHS advises REACH ACO’s contact the beneficiary or the provider’s office to clarify or inquire about additional language options that would be acceptable to the beneficiary.
3. CMS does not impose any HEDR collection requirements. REACH ACOs may leverage any data source to collect HEDR data, including, but not limited to, provider EMRs, care management assessments and beneficiary surveys. CHS advises REACH ACOs to leverage the available provider EMR data as a starting point for an assessment of the completeness and admissibility of demographic and SDoH data for HEDR submission. If the REACH ACO needs additional data, CHS advises the REACH ACO work with the PCP offices to update office visit questionnaires, care management assessments and distribute surveys to beneficiaries to ensure required demographic and SDoH data fields are captured.
4. REACH ACOs may submit its PY23 HEDR data at any time from mid-January to mid-March 2024. CMS clarified this in the October 3rd ACO REACH newsletter after two prior announcements offered differing HEDR submission timeframes. Originally, CMS announced four singular PY23 HEDR submission dates: 7/1/2023, 10/1/2023, 1/1/2024, 4/1/2024. In the spring, CMS then pushed the PY23 HEDR submission timetable back and announced a continuous submission window open from late summer 2023 to April 2024. CMS will also provide feedback on each HEDR submission, providing REACH ACOs with opportunities to address data issues in prior submissions without penalty.
5. CMS will accept HEDR submissions through a Health Data Reporting (HDR) application that has not yet been released. The HDR application will be separate from 4innovation (4i), the ACO REACH portal housing all ACO REACH knowledge and nearly all other ACO REACH submission. CMS will publish an HDR portal implementation guide for REACH ACOs to read and interpret prior to the end of October and subsequently host several HEDR submission webinars. While the go-live date of the HDR application has not been released, based on current and available information, the HDR application should be live prior to the HEDR submission window in mid-January 2024.
If you are interested in learning more about or obtaining support with ACO REACH, please reach out to us at info@copehealthsolutions.com or 213-259-0245 to learn about how CHS can help your organization succeed in this CMMI model, MSSP ACO or any other form of value-based payment for Medicare, Medicaid or commercial lines of business.

