On January 9, 2017 the Washington Healthcare Authority (HCA) reached a pivotal milestone in their partnership with the Centers for Medicare and Medicaid (CMS) to transform the delivery and quality of care served to their Medicaid population. The two parties finalized the Standard Terms and Conditions (STCs) of the 1115 Medicaid waiver, making the waiver officially approved, which up until that point had only been agreed-in-principle at the federal level. The STCs are an essential document as they outline the fundamental rules and regulations that HCA, the regional Accountable Communities of Health (ACHs) and providers throughout the state will have to follow as they begin to implement the transformation elements outlined in the waiver.
Over the coming months, HCA will develop the remaining governing documents of the waiver known as the protocols (or attachments to the STCs) and work to gain approval of these from CMS. These documents are critical as they will further define items such as:
- Project valuation and the funds flow formula that will allocate the maximum dollars each ACH can earn through demonstrated performance
- The semi-annual reporting requirements needed to demonstrate performance
- Expectations around the collection and reporting of clinical quality outcomes
- A number of other key governing regulations.
While the STCs are not complete until all of the protocols are developed and approved, this Health Insights piece will focus on five key terms outlined in the STCs related to the DSRIP program and offer suggestions as to things ACHs and community providers should begin to consider as they prepare for the implementation requirements of waiver participation. This piece is not intended to prescribe waiver next steps or compare other waiver programs; COPE Health Solutions has developed other thought leadership pieces that explain these elements of the Washington waiver and those articles are linked at the bottom of this piece.
STC Terms to Monitor
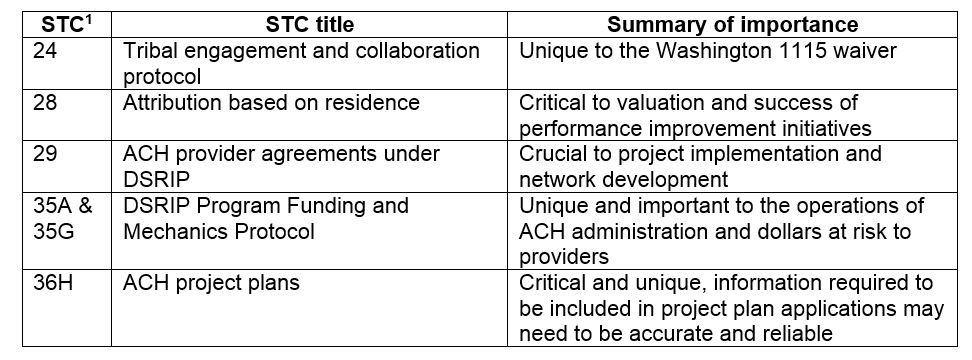
STC 24 Tribal engagement and collaboration protocol
This regulation defines the expectation that ACHs will be expected to adopt a collaboration and communication policy with all tribes and Indian Health Care Providers (IHCPs) in their geographic region. ACHs will be required to collaborate and communicate in a timely and equitable manor with tribal stakeholders and receive ongoing training on Indian health care delivery. To date, Washington state is unique in this requirement of heightened collaboration and cultural competency with tribal communities and providers. While this may represent an additional challenge for ACH governing bodies and HCA across the state, it presents a special opportunity to showcase best practices and solutions for collaboration and demonstrating improvements in a defined demographic within the state. ACH governing bodies and administrative leadership will need to be prepared with innovative ideas for collaboration and ongoing engagement with tribes and IHCPs in their area and incorporate the training requested in the STCs in their operational budgets and staffing plans.
STC 28 Attribution based on residence
The Washington waiver will not be the first waiver to attribute individuals to regional Medicaid service areas and providers but it is an important condition. It will likely impact the maximum valuation ACHs are eligible to earn over five years and will also define the individuals each ACH is measuring to determine their level of improvement for population health measures. The use of attribution also signals that HCA may be a source of data and analytics for ACHs in the measurement and reporting of clinical quality measures since performance will be based on a set of pre-defined members.
There will be more information around attribution and its links to performance measurement when the protocols are released but this could mean a reduced reporting burden on ACHs and their providers if HCA is able to leverage claims databases or another set of clinical data. The potential downside to the use of claims data is the likelihood of a significant time lag in receiving information and the possibility of being measured for performance on data that may pre-date regional improvement implementation activities.
STC 29 ACH provider agreements under DSRIP
STC 29 reads “In addition to the requirements specified in the DSRIP Program Funding and Mechanics (PFM) Protocol (Attachment D), ACHs must establish a partnership agreement between the providers participating in projects.” It is anticipated that the PFM may further outline requirements of these provider agreements in addition to funds flow stipulations. ACH leadership and governing bodies should be prepared for a range of possibilities and responsibilities associated with the required provider agreements under STC 29. These agreements may just be a formality of partnership and participation between the ACH organization and community providers. Or, the agreements may need to be complex and include the definition of provider roles and responsibilities in project and transformation activities, and specify performance milestones and metrics that a provider must complete in order to earn a specific amount of funds.
Understanding the requirements of this protocol will be imperative as it may define a large workstream and focus for ACH organizational leadership over the five years of the waiver. COPE Health Solutions is experienced in network development, designing and implementing provider performance based contracts in a DSRIP environment. Our team can partner with ACH organizational leadership to define your contracting strategy, develop the right network of providers and ensure the provider agreements set the ACH up for success under DSRIP and in preparation for operating within the constructs of value-based payment agreements in the coming years.
STC 35A & 35G DSRIP Program Funding and Mechanics Protocol
More information regarding semi-annual reporting for payment, along with more information for the required quarterly reports ACHs must submit to the state, is expected when the protocols are fully developed. For now, the STCs point to two different on-going reporting requirements that ACH organizations and their leadership need to be prepared for.
STC 35A stipulates that the state must develop a standardized form for ACHs to update their progress and performance on metrics on a quarterly basis (STC 37A discusses the minimum semi-annual review for payment that will occur based on ACH reports). Protocols will likely further define the official number of reports required per year, the required contents of those reports and how often those reports are reviewed for approval of payment based on performance. What is important for ACH leadership and their providers to understand regarding this STC in particular is that developing and implementing a successful reporting strategy will be imperative for the success of the ACH. Reports will be used to demonstrate progress and achievement and the state and CMS will substantiate payment to the ACH and its providers based on this documented achievement. Quarterly reporting can place a heavy burden on ACH staff and participating providers as it requires a high level of effort and a strategic operational plan to efficiently and effectively report each quarter. COPE Health Solutions is deeply experienced in developing and implementing successful reporting structures, shown in our above 94% draw down of eligible funds for clients in other national DSRIP programs.
Having a portion of funds at risk statewide is something other DSRIP programs have seen, but the requirement in STC 35G “… for DSRIP years 4 and 5, all incentive dollars are contingent upon the state achieving fully integrated managed care by January 2020 for physical and behavioral health services” is a unique requirement to the Washington waiver. Other states have seen a portion of year 4 and 5 dollars at risk for achieving a population health outcome such as reduced readmissions but this is the first waiver to put all incentive dollars at risk for a statewide initiative to fully integrate physical and behavioral health. ACHs and their providers will need to be well aware of this requirement and ensure that they are taking all of the necessary steps to meet the outlined requirements and timeline protecting the incentive dollars for all providers in the state in years 4 and 5 of the waiver.
STC 36H ACH project plans
The official project plan template is anticipated to be released at the end of May 2017, and ACHs will likely have the summer and early fall to coordinate and collaborate with their network providers to select their projects, outline budgets and develop a plan for sustainability. Based on the STCs, it is understood that project plans will be scored and evaluated, which may result in a factor in the valuation formula for maximum funding (in addition to attribution) that each ACH may be eligible to earn over five years.
All DSRIP programs require an initial project and implementation plan, but what is interesting in Washington STC 36H is “The initial ACH Project Plan must include baseline data on all applicable quality improvement and outcome measures”. The inclusion of baseline data could present a large challenge to ACHs and their providers to collect accurate data in a short time frame across a large number of independent clinical providers and community based organizations. In DSRIP programs, baseline data is used as the initial benchmark that future success, and payment, will be measured against. It is unclear based on the STCs what exact baseline data will be required in the project plans, but this is a significant requirement ACH organizations should pay close attention to. To the extent possible ACHs should try and understand from HCA what baseline information is anticipated to be required in the project plan applications prior to the release of the template later this year. ACHs should begin thinking about a strategy to collect, aggregate and verify data from their network providers based on the timeframe required for project plan submission in late 2017.
About COPE Health Solutions
COPE Health Solutions is a leading national health care consulting firm with extensive experience with 1115 waivers and DSRIP. We specialize in the key steps to sustainability such as assessing current state, planning and executing transformation projects. With a corporate office in Seattle, in addition to New York and our flagship office in Los Angeles our team is filled with a diverse range of subject matter experts that can assist Accountable Communities of Health and their providers be successful in a DSRIP program and ultimately sustainable in a value-based payment environment. Currently we are looking forward to opportunities to assist ACHs with project selection, project plan development and submission and budget planning, as those are the first, and very imperative, steps towards waiver implementation in Washington. For more information, please contact info@copehealthsolutions.com.
Health Insights related to the Washington waiver and the importance of strategic waiver implementation
- Building the Core Elements of an Accountable Community of Health to Support 1115 Waiver implementation
- The Role Of Medicaid Waiver Transformation Projects In Transforming The Core Strategic And Business Planning Framework Of Health Care Organizations
- Washington State Global 1115 Waiver: An Overview
Footnotes:
1 http://www.hca.wa.gov/sites/default/files/program/Medicaid-demonstration-terms-conditions.pdf