The New York State Department of Health (NYSDOH) recently released a draft proposal to extend its Delivery System Reform Incentive Payment (DSRIP) program as part of the state’s 1115 Medicaid waiver, currently set to expire at the end of March 2020. Asking the Centers for Medicaid and Medicare Services (CMS) for $8 billion over four years additional years, the proposed extension would significantly shift the course of DSRIP, if approved. As the future of the DSRIP program remains uncertain, performing provider systems (PPS) are faced with a number of opportunities to consider.
 CMS Response
CMS Response
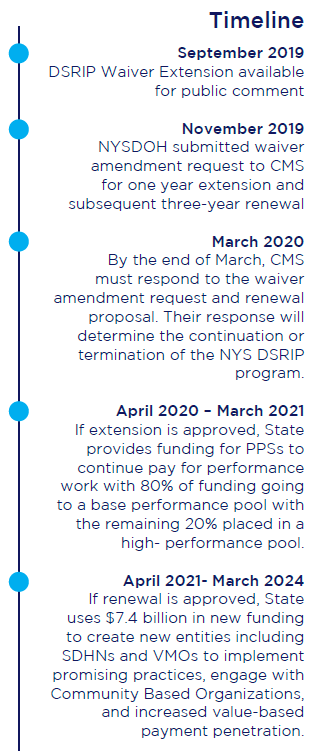
By March 31, 2020, CMS must formally respond to NYSDOH’s waiver amendment. While there are a number of possibilities as to how they may respond, broadly the options are below:
- Approved – CMS approves both extension and renewal, starting the extension year in April 2020 and renewal from 2021-2024.
- Amended – CMS approves parts of extension or renewal resulting in a new NYS DSRIP program. This negotiation could result in a delay of implementation beyond April 2020.
- Denied – CMS denies both extension and renewal, resulting in the end of the NYS DSRIP program, or at least the federal funding. Even if the waiver is not extended or renewed by CMS and federal funding of DSRIP ends, the policy changes described in the waiver application by NY State are still likely to be enacted programmatically.
Opportunities for PPSs
Regardless of CMS’ response, PPSs have multiple opportunities to align with state priorities and prepare for increased value-based payment penetration. Considerations should include:
- Examine Existing Network – With the clinical performance data gleaned through four years of DSRIP, PPSs have the opportunity to continue relationships with high-performing partners and consider removing partners with either low performers or partners unwilling to invest to make clinical improvements. Identifying high and low performers and strengthening relationships with top performers will prepare PPSs for contracting in the renewal period should the amendment be approved.
- Expand Network – PPSs should also consider expanding their network by adding more primary care providers (PCP). NYSDOH plans to move towards a more traditional attribution model in the renewal, making PCP attribution critical to receiving a larger award. Federally qualified health centers and IPAs will be key partners for attribution, advancing clinical programs and meeting performance measures.
- Planning Governance – The State has made clear that they want PPSs to expand to include a broader range of stakeholders in their governance, including CBOs and MCOs in voting roles. PPSs can use this time to plan for governance changes, including updates to committee structures and rosters.
- Social Determinants of Health – Given the State’s growing interest in social determinants of health (SDOH) and the potential to create Social Determinant of Health Networks (SDHNs), PPSs can begin to understand which non-clinical areas their members are lacking access, as well as expanding relationships with Community Based Organizations (CBOs). Key areas include housing and food insecurity, interpersonal violence, transportation and toxic stress.
For more information, please contact Brian Ball, Manager, COPE Health Solutions at bball@copehealthsolutions.com or call (213) 444-9738.

