Introduction
Since March of 2020, the entire health care system supply chain has been disrupted due to the impact of the Covid-19 pandemic. Stay-at-home orders, unemployment and a surge of Covid-19 patients suppressed outpatient volumes, acutely altered payer mix and constrained hospital capacity. Fee-for-service (FFS) primary care was hit especially hard by this seismic shift in the market, with volumes plummeting, taking cash and revenues with it. One report cites an average 60 percent decrease in volumes and a corresponding 55 percent decrease in revenues.1
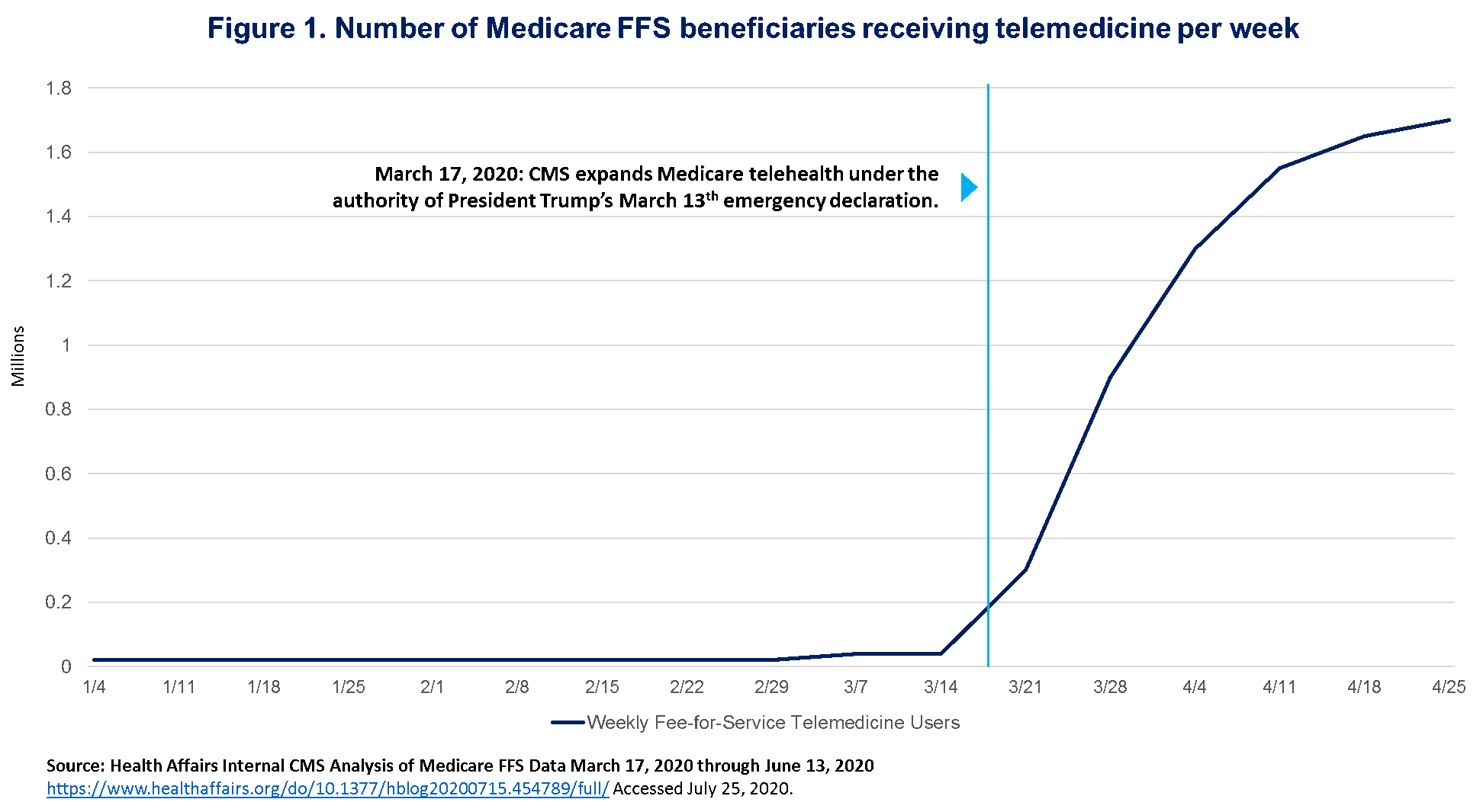
FFS remains the keystone of the majority of payment models, including the underlying chassis of most advanced payment models (APMs), leaving the United States health care system vulnerable to such disruption. Likewise, regulations that constrain sites of care in order to be reimbursed have prevented providers from migrating lower acuity treatment to lower cost, or even virtual care settings. As the crisis crescendoed, providers sought new ways to keep their patients safe and engaged, as evidenced by the explosive uptake of telehealth and remote care models (Figure 1). Telehealth is not new; however, payment and regulatory barriers have inhibited widespread care model innovation and adoption. The last few months have demonstrated that if given financial and regulatory flexibility, providers are well-equipped to deploy new care modalities while still maintaining safety and quality of care. This calls into question the current care models and signals a need for reform as a means to improve access, efficiency and longitudinal outcomes.
Physician compensation models ultimately determine the contours of care delivery; financial sustainability and regulatory compliance set the guardrails within which care models are designed and in turn optimized. Physicians will seek to provide the best care they can afford to offer; if we want innovative care delivery, we must first address the question of compensation.
It is no wonder that providers under capitation weathered this storm much better,2 as their payment model had provided them with consistent cash flow affording them the opportunity to be early adopters of new modalities like telehealth and to direct funds to address social determinants of health (SDOH). Capitation gives physicians the flexibility to redesign their care models and the agility to deploy innovative interventions, without disrupting reimbursement, and further promoting quality of care.
Misaligned Compensation Models and Half-Built Population Health Infrastructure
Today, most physicians are reimbursed variably across lines of business, with a significant portion of revenues reliant on volumes, and some incentives tied to value – yet a small percentage of overall compensation. This makes fully embracing a value-based care model financially untenable. That said, some infrastructure has been established to support the select value-based payment (VBP) initiatives underway. True risk-based payment models call for population health management infrastructure, which requires up front capital to build – capital currently funneled through FFS revenue streams. As a result, many providers have found themselves caught between differing priorities.
Further, Covid-19 demanded the market acutely respond, straining FFS business models as that supply chain was disrupted by the necessity of stay-at-home and distancing requirements – many to the point of bankruptcy or closure3 – and forcing providers to seek ways to engage their patients while saving their businesses. Misaligned payment models were temporarily alleviated through regulatory and financial relief efforts. What has resulted is an “ad hoc” large-scale case study on the merits of innovative care delivery models, namely telehealth and home-based care delivery, often enhanced with community-based wraparound services to address SDOH.
As a direct result of this rapid market-wide pivot, a patchwork of new infrastructure has been deployed. However, the payment models that support them are both temporary and incomplete. The rapid deployment also means speed was prioritized at the expense of efficiency and comprehensiveness, calling for further investment to fill gaps and optimize new infrastructure. Taking a systems-level view, physicians find themselves operating with several misaligned payment models, sitting on new infrastructure and revised care models, low cash on hand, and continued uncertainty. These conditions are ripe for re-examination of overall organizational health and strategy. As part of this effort, physician organizations should take this moment to refresh, or establish, their Value-based Care Roadmaps.
Building Organizational Resilience – What You Can Do Today
The needs for which providers developed Covid-19 interventions do not appear to be going anywhere – and in fact many existed before the current crisis. Covid-19 has in many ways exposed existing limitations and amplified shortcomings of the current health care system, forcing our hand toward reform. We have passed this critical threshold and must continue forward toward compensation models that support value-based care delivery and build resilience against the inevitable future crisis. To strategically advance their Value-based Care Roadmap, organizations should take the following five steps:
- Conduct a current state capabilities gap assessment to understand best practice care model and population health infrastructure
- Perform data analytics to get a handle on clinical and financial performance across various populations and risk or acuity levels
- Align physician compensation and incentives with value-driven care
- Review overall clinical and contractual affiliations to best position your services in a value-based healthcare community
- Identify programs to expand risk, move upstream on the premium dollar, and improve cash flow to fund needed investments
Timely Opportunities – The Benefit of Acting Now
Most organizations are understandably in survival mode, leaving little room for strategy and vision setting. However, there is often an opportunity in crisis. Physicians should take advantage of existing opportunities for loans and grants, such as the Economic Injury Disaster Loans (EIDL) through the Small Business Administration (SBA). Another timely program is Medicare Direct Contracting (MDC), which is an ACO-like program that provides a glide path to capitated risk. As it pertains to physician practices, MDC offers opportunities for primary care physician (PCP) capitation, reimbursed at seven percent of the total cost of care and reconciled to benchmark at the end of the performance period. This offers a frontloaded payment structure that provides cash flow required for needed investments. The next application for MDC comes out first quarter of 2021, leaving enough time to get started on Value-based Care Roadmap work in the fall and developing a strategy to leverage MDC – and other programs – in funding population health infrastructure.
For more information on physician alignment, VBP Roadmaps and Medicare Direct Contracting, contact Andrew Snyder, MD, Principal & Chief Medical Officer of COPE Health Solutions at asnyder@copehealthsolutions.com or 401-225-9417 or Shanah Tirado, MBA, MPA, Manager of COPE Health Solutions at stirado@copehealthsolutions.com or 213-369-7415.
Endnotes
1 https://www.mgma.com/getattachment/9b8be0c2-0744-41bf-864f-04007d6adbd2/2004-G09621D-COVID-Financial-Impact-One-Pager-8-5×11-MW-2.pdf.aspx?lang=en-US&ext=.pdf Accessed July 25, 2020.
2 https://www.modernhealthcare.com/insurance/covid-19-may-end-up-boosting-value-based-payment Accessed: July 25, 2020.
3 To date, there has been a loss of access to over 40% of family physicians driven by practice closures. https://healthlandscape.org/covid19/ accessed: July 25, 2020.

