Background: Benefits of a Post-Discharge Phone Program
Hospitals have improved patient outcomes and patient satisfaction scores via implementation of a successful post-discharge phone call program to achieve:
- Improved patient outcomes:
- Patients receiving a post-discharge call were 23.1% less likely to be readmitted compared to patients who did not receive a call1.
- Early detection of adverse events and more rapid problem resolution:
- Out of 40,000 individuals interviewed during a post-discharge call, 21% reported an adverse event or problem2, which was able to be addressed and resolved.
- Higher patient satisfaction scores:
- There is a strong association between post-discharge calls and “likelihood-to- recommend the hospital” rating on a Press Ganey survey3.
A combined decrease in hospital readmissions and increase in Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores positively affects a hospital’s Value Based Purchasing score and reduces payment penalties for readmissions.
The benefits of reconnecting with patients post discharge are clear; however, allocating adequate resources to ensure a successful, formal post-discharge phone calls process has been a struggle for most hospitals.
The Problem
The most common barriers to establishing a formal post-discharge phone calls process are:
a) Resistance from nursing staff to take on an additional task, and
b) Lack of structured training for conducting post discharge calls
St. Francis Medical Center (SFMC) in Lynwood, CA experienced these barriers when hardwiring the post-discharge phone calls process on inpatient units. However, it pursued a different approach — a solution which has sustained positive results over the 5-month period since implementation.
The Solution
SFMC partnered with COPE Health Solutions’ Health Scholar Program* to first increase the number of post-discharge phone calls made (percent of calls attempted) and subsequently, increase the number of patients actually interviewed (percent of calls completed).
The initial goal of Health Scholar involvement in the post-discharge phone calls process was to jumpstart the process for inpatient units towards achieving a 100% attempt rate during the implementation phase.
Nine out of 320 CCEs from SFMC’s Health Scholar Pipeline were selected to participate in the initiative under direct supervision from nursing staff. Selected Health Scholars received a 3-hour training from SFMC’s Patient Advocate/Satisfaction Coordinator and completed a training competency checklist signed off by SFMC’s trainer. Health Scholars initiated all post-discharge phone calls by following a pre-approved script and forwarded all calls requiring clinical intervention to the nursing staff.
Results
Health Scholars were able to jumpstart the discharge phone calls process for four units – 7th, 6th, 4th floors and 2 East. Figure 1 indicates the catalytic effect of Health Scholar presence on achieving 100% attempt rates – all units on which Health Scholars assisted with the discharge phone calls process reached a 100% attempt rate within 3-4 months of implementation compared to units without Health Scholars. St. Francis Medical Center has benefited from an already-existing resource (Health Scholars) by reaching successful results more rapidly.
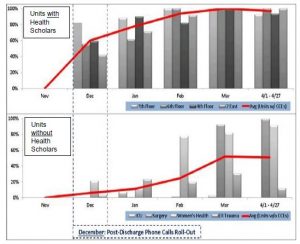
Figure 1: Average % Attempt Rates for Units with Health Scholars vs Units Without Health Scholars
Conclusion
The post-discharge phone calls initiative, in partnership with St. Francis Medical Center and COPE Health Solutions, resulted in a faster yield of 100% attempt rates for units that utilized Health Scholars compared to units that did not have Health Scholars. This unique solution indicated that Health Scholars are a resource on which the hospital could depend to rapidly produce successful results, especially in the first phases of initiative implementation with hospital staff. This study will be revisited after Health Scholars begin attempting post-discharge calls on hospital units that experienced a less rapid success rate at St. Francis Medical Center.
Footnotes:
1 Patricia L. Harrison, MPH et. al. “The Impact of Postdischarge Telephonic Follow-Up on Hospital Readmissions.” Population Health Management (2011 ): 27–32 <http://www.ncbi.nlm.nih.gov/pmc/articles/PMC 3128446/>.
2 Louden, Kathleen. SHM 2009: Postdischarge Adverse Events Are Common, But Not as Common in Elderly. May 2009. April 2013.<http://www.medscape.com/viewarticle/703131>.
3 David A. Guss, MD et al. “The Impact of Post-Discharge Patient Call Back on Patient.” The Journal of Emergency Medicine (2013): 236– 241.<http://www.emergencyexcellence.com/impact ofpatientcallbacksJEM.pdf>.

