The Centers for Medicare & Medicaid Innovation has laid out a new framework for driving health system transformation over the next 10 years. While CMMI did not announce specific changes or new programs as of yet, the focus on value-based care, aligning financial incentives through value-based payments and health equity — and making more progress faster — is clear.
The strategic refresh follows months of review by the Biden Administration of more than 50 alternative payment models (APMs) piloted since CMMI’s founding in 2010. It found that six programs showed statistically significant savings while others have yet to be in place long enough for complete analysis.
CMMI identified opportunities for improvement that it plans to address going forward including a lack of diversity among participating beneficiaries, complex payment policies and model overlap rules that create a heavy administrative burden. CMMI also cited a lack of provider tools for managing cost and risk, need for significant infrastructure investments and complex financial benchmarks that limited savings and effectiveness as barriers to success that must be overcome.
Going forward
Taking these and other lessons from the first decade to heart, CMMI plans to make future programmatic decisions with five strategic objectives in mind:
- Drive accountable care.
- Advance health equity.
- Support care innovations.
- Improve access by addressing affordability.
- Partner to achieve system transformation.
CCMI points to the following programs in 2021 that reflect its goals:
- Advancing Health Equity: Community Health Access and Rural Transformation Model
- Accountable Care: Initial cohorts for Primary Care First (PCF) and Global/Professional Direct Contracting (GPDC)
- Accountable Care: ESRD Treatment Choices Model
- Addressing Affordability: Part D Senior Savings Model
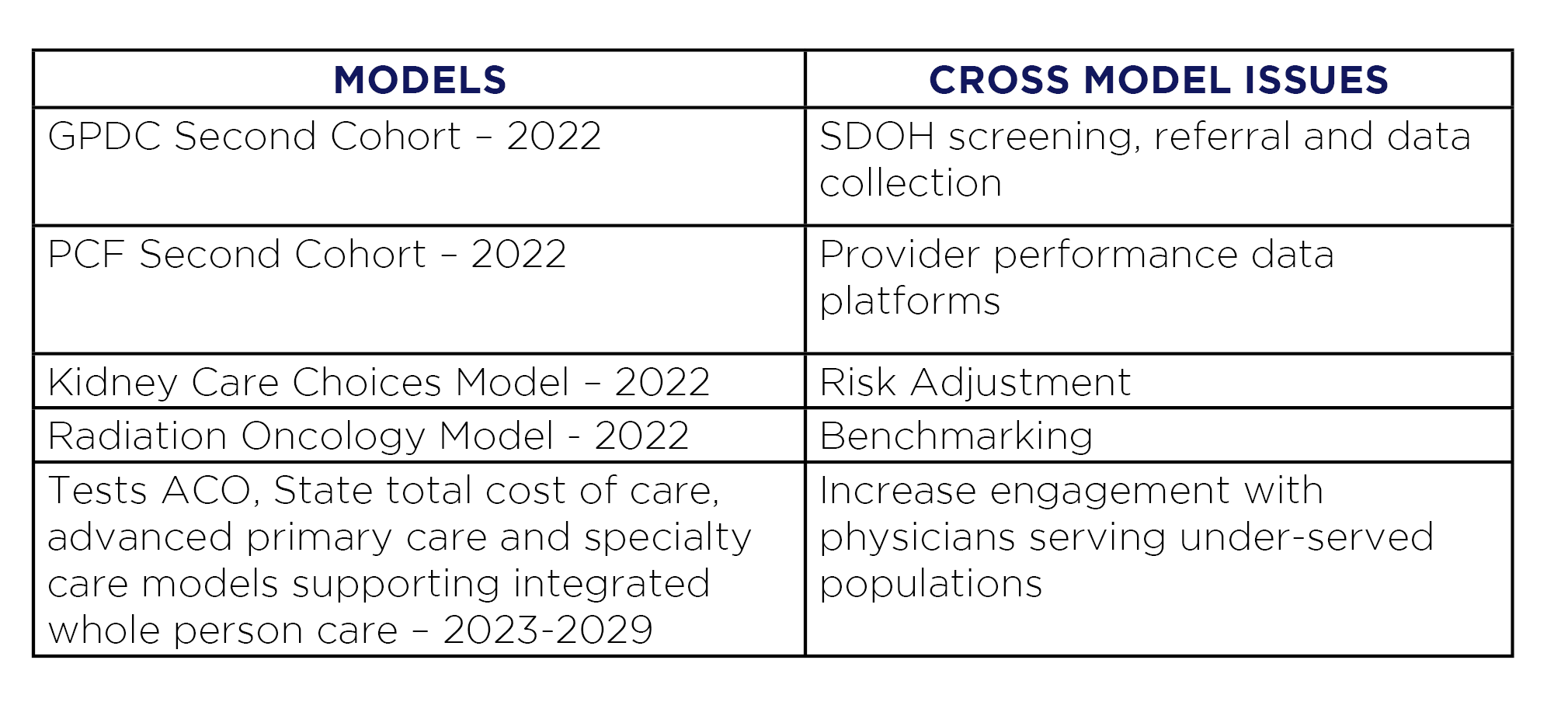
CMMI also shared examples of models and cross-model issues it may focus on in 2022 and beyond to advance its strategy and inform transformation:
While more specifics will be announced in the months ahead, CMMI has articulated a strong vision for the next decade. Here are five things to know:
1. Fee-for-service as a primary payment mechanism has an expiration date. CMMI wants every Medicare fee-for-service beneficiary and the vast majority of Medicaid beneficiaries in care programs that are accountable for quality and total cost of care by 2030.
2. Expect tighter coordination between Medicare and Medicaid.
3. Social determinants data gathering and integration into analytics will be non-negotiable. For more information on a path forward, see our article in this issue about leveraging Z codes.
4. Patient experience will be a key part of care innovation metrics.
5. CMS may absorb more costs to encourage beneficiaries to access high-value treatment.
Still, nothing is carved in stone quite yet. As part of its effort to partner for system transformation, CMMI is hosting a series of listening sessions, starting in November, about its new framework, objectives and related issues with beneficiaries, health equity experts, primary care, safety net, specialty providers, states, and payers. This will be an important opportunity to help shape CMS programs for years to come.
For more information, contact info@copehealthsolutions.com.

