On January 9, 2024, CMS approved an amendment to New York’s Medicaid 1115 Waiver, allowing the state to make investments in Medicaid initiatives that expand access to primary and behavioral health, address health-related social needs (HRSN) to reduce disparities and promote health equity, and strengthen the healthcare workforce. The term of the demonstration amendment will run through March 31, 2027.
Through this innovative waiver amendment, New York State (NYS) is aligning itself with CMS goals and new programs to promote value-based payment (VBP) strategies through two Center for Medicare and Medicaid Innovation (CMMI) models: Making Care Primary (MCP) for upstate New York and States Advancing All-Payer Health Equity Approaches and Development (AHEAD) for downstate New York.
One of the main initiatives in the waiver amendment is a Medicaid Hospital Global Budget. The goal of this initiative is to invest in safety net hospitals to propel them towards success in population health.
There are five things to know regarding available funding, eligibility, and requirements to participate in this initiative:
1. The amendment stipulates that the state will receive up to $2.2 billion over the demonstration amendment term, or $550 million annually, to invest in safety net hospital readiness for success in Medicaid Global Budgets and potentially the AHEAD program.
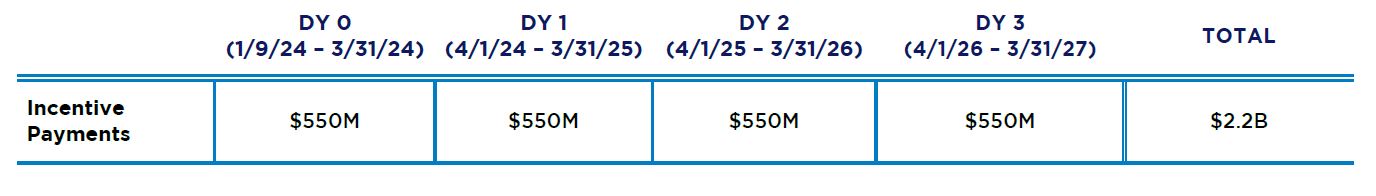
Incentive payments under the Medicaid Hospital Global Budget Initiative are not considered patient care revenue nor offset against disproportionate share hospital expenditures or other Medicaid expenditures that are related to the cost of patient care – new money invested in safety net hospital transformation.
2. Safety net hospitals must meet the following eligibility criteria to participate:
- Private Not-For-Profit ownership structure
- Located in Bronx, Kings, Queens or Westchester county
- Medicaid and Uninsured Payor Mix of at least 45%
- Average operating margin ≤ 0% over CY19-22 based on audited Hospital Institutional Cost Reports (excluding COVID-19 relief funding and state-only subsidy)
- Hospital (or affiliates) received state-only subsidies due to financial distress in FY 23 and/or 24
3. NYS must submit a Medicaid Global Budget implementation plan through either the new CMS States Advancing All-Payer Health Equity Approaches and Development (AHEAD) program or independently.
- AHEAD model is scheduled to operate for 11 years, from 2024 – 2034. States applying to AHEAD will be required to select one of three cohorts depending on readiness to implement the model:
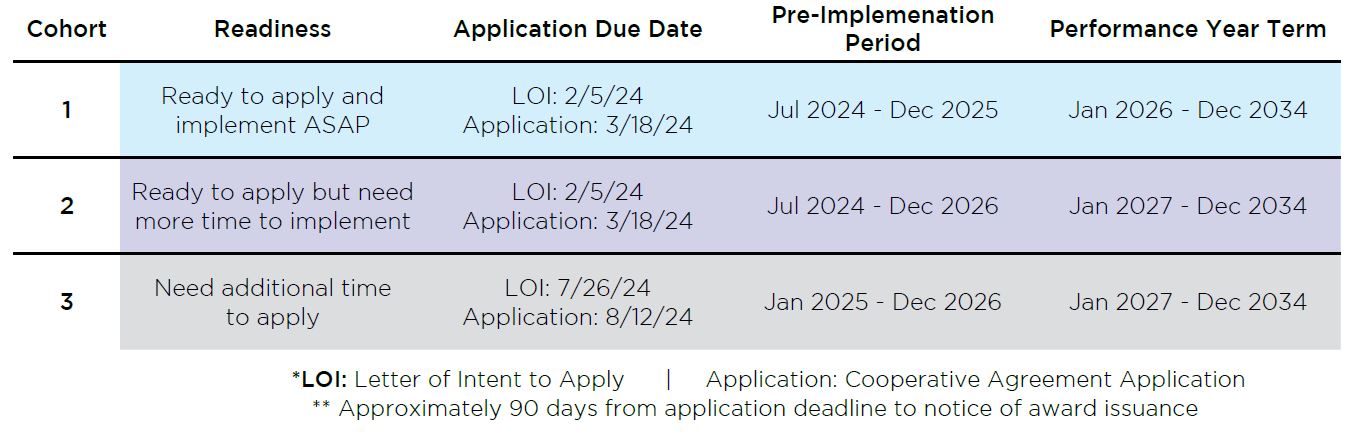
- NYS may apply to either of the three Cohorts to satisfy the requirements of the 1115 Medicaid waiver amendment
Key Action Item: Participating hospitals will need to submit an LOI expressing intent to participate in a CMS model or another global payment model by March 31, 2024.
- If NYS applies to Cohort 3, hospitals must reconfirm via an LOI that is will participate in the hospital global budget as part of the AHEAD model
4. Participating hospitals must submit a common fact base and a custom roadmap to the state by March 31, 2025 with key targeted activities to transition to a global budget model
- Common fact based information examples:
- Key statistics on population served, degree of patient engagement/satisfaction;
- Competitive landscape, including payor/provider and regulatory impacts;
- Overview of current financial performance and payment models;
- Evaluation of IT infrastructure, interoperability capabilities, data infrastructure, and reporting and analytics capabilities;
- Evaluation of physical plant infrastructure and necessary capital investments to support population health
- Assessment of historical/projected operating expenses with specific focus on variable and non-variable expenses; and
- Opportunities for quality improvement.
- Custom roadmap minimum required activities:
- Data, interoperability, analytics, and reporting
- Financial modeling
- Care coordination and management
- Quality improvement
- Compliance and business operations
- Network and physician engagement
- Patient experience and engagement
- Opportunities for service line rationalization based on community need
- Leadership, governance, and talent change management
5. Participating hospitals must also submit a health equity plan to the state by March 31, 2025, complete with quality/equity measures, including, but not limited to:
- Pay for Performance (P4P) quality measures
- Measures that align with CMS’ Disparities-Sensitive Measure Set
Hospitals must also submit complete quality data on metrics yet to be specified by the state.
In Demonstration Year 2 (ending March 31, 2026), participating hospitals must submit quality measures and execute on their custom roadmaps.
In Demonstration Year 3 (ending March 31, 2027), participating hospitals must provide a progress report and, where appropriate, updates to their roadmaps to the state for approval. In addition, hospitals (and the state) must submit achievement on the initiative’s incentive metrics.
Key Considerations:
1. Safety net hospitals can leverage the funding available to build capabilities and infrastructure that will support success in both global budget and in wider risk-based arrangements with payers, as well as self-insured employ plans.
Irrespective of whether safety net hospitals participate in either the NYS 1115 Medicaid waiver amendment’s or the CMMI AHEAD model’s global budget initiative, there will be payors and lines of business that are not included within global budgets.
Safety net hospitals have an opportunity to leverage their roadmap for global budget initiatives and apply the infrastructure they build to succeed in more global risk arrangements overall.
Hospitals will need to assess gaps in current infrastructure, including physician networks, population health management and contracting that will need to be closed to set up for success under both global budgets and value-based payment agreements with payers.
2. Partnerships with community IPAs can improve performance in global budgets and other risk arrangements.
Safety net hospitals should consider configuring or reconfiguring their relationships with community IPAs that are successful at managing risk both inside and outside the hospital facility, as these groups can assist hospitals in managing populations in both value-based payment agreements and global budget initiatives. Various large physician groups and/or IPAs currently operate as clinically integrated networks (CINs), and such networks have already built significant infrastructure to help manage population health and reduce utilization of acute services.
If you are interested in learning more about the waiver or how your organization can participate, please reach out to Allen Miller at amiller@copehealthsolutions.com or 213-542-2234, Steven Hefter at shefter@copehealthsolutions.com or 213-660-6081 or
Patrick Pilch at patrick.pilch@ankura.com or 516-301-1470.
We are excited to meet with you and learn how CHS can help your organization succeed in value-based payment for Medicare, Medicaid or commercial lines of business.


