Medicaid membership has grown dramatically over the past decade, even with the recent dips due to fall-off from post Public Health Emergency redetermination, however Medicaid reimbursement has not kept up with inflation. Health systems and other providers are in a very tight spot with increasing costs driven by staffing, supply chain, the need to transform to impact population health and access, and the need to catch up with often delayed infrastructure maintenance. We will explore here three proven approaches to optimizing Medicaid revenue and quality:
- Establish and strengthen partnerships with existing FQHCs in the market
- Transition existing high Medicaid volume clinics to an FQHC model
- Maximize Medicaid managed care contracting strategy
Below we provide a high-level overview of the three strategies, which can be pursued independently or together.
FQHCs as Key Partners and Contracted providers in an IPA, CIN or ACO
FQHCs are uniquely poised to serve not only Medicaid, but also low income Medicare, dual eligible, subsidized exchange and uninsured patients. The primary care, dental, optometry, podiatry and other specialty care provided by FQHCs, supported by their PPS wrap-rate, can reduce frequency of unnecessary emergency visits and acute hospitalizations and improve quality scores. This makes FQHCs a great partner for health systems and IPAs, CINs or ACOs that are in or evaluating risk arrangements.
FQHCs have a mission to serve the community and receive enhanced reimbursement based on actual costs to offer critical care coordination services (interpretation, transportation, health education, care management and sliding fee scales) that address key SDoH needs and are key to reducing cost and improving quality. Partnerships with existing FQHC’s can be developed or strengthened by:
- Including FQHC’s in existing IPA networks, giving the FQHC access to MSO services and value-based or at least quality upside arrangements
- Strengthening of discharge and transitions of care programs that recognize the value of FQHC services and support patient connections to these services
- Understanding and addressing FQHC pain points, such as access to high quality specialty care – this may include having some specialists see patients part or full time in FQHCs where there is a higher reimbursement opportunity
Transitioning Existing High Medicaid Volume Clinics to FQHC Models
Health systems and medical groups or IPAs with existing clinics serving high-volume Medicaid populations may be uniquely poised to transition to an FQHC model. While a transition to an FQHC model will involve operational change, there are several upsides for all involved:
- Improved revenue for the clinics for both Medicaid and Medicare under the cost-based prospective payment system (PPS) rate
- Improved quality with additional care coordination services that FQHCs are funded to provide
- Reduced need to subsidize money-losing clinics through revenue flowing back through a management services and/or professional services agreement with the FQHC
There are four models that can be considered for FQHC transition of existing clinic sites, as described in the table below. Organizations considering a transition should be sure to do so with a full understanding of the benefits, governance structure and FQHC requirements under each model to ensure the transition is successful and to maintaining desired alignment, value based payment contracting participation and care coordination in the long term.
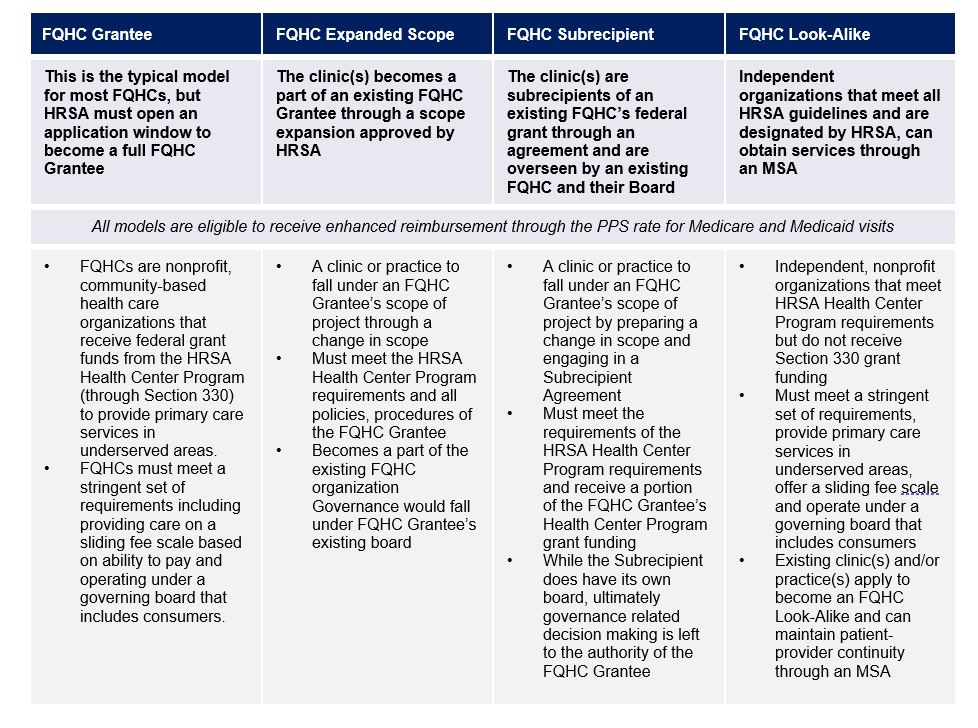
FQHC Grantee FQHC Expanded Scope FQHC Subrecipient FQHC Look-Alike
This is the typical model for most FQHCs, but HRSA must open an application window to become a full FQHC Grantee The clinic(s) becomes a part of an existing FQHC Grantee through a scope expansion approved by HRSA. The clinic(s) are subrecipients of an existing FQHC’s federal grant through an agreement and are overseen by an existing FQHC and their Board Independent organizations that meet all HRSA guidelines and are designated by HRSA, can obtain services through an MSA
All models are eligible to receive enhanced reimbursement through the PPS rate for Medicare and Medicaid visits
- FQHCs are nonprofit, community-based health care organizations that receive federal grant funds from the HRSA Health Center Program (through Section 330) to provide primary care services in underserved areas.
- FQHCs must meet a stringent set of requirements including providing care on a sliding fee scale based on ability to pay and operating under a governing board that includes consumers.
- A clinic or practice to fall under an FQHC Grantee’s scope of project through a change in scope
- Must meet the HRSA Health Center Program requirements and all policies, procedures of the FQHC Grantee
- Becomes a part of the existing FQHC organization Governance would fall under FQHC Grantee’s existing board
- A clinic or practice to fall under an FQHC Grantee’s scope of project by preparing a change in scope and engaging in a Subrecipient Agreement
- Must meet the requirements of the HRSA Health Center Program requirements and receive a portion of the FQHC Grantee’s Health Center Program grant funding
- While the Subrecipient does have its own board, ultimately governance related decision making is left to the authority of the FQHC Grantee • Independent, nonprofit organizations that meet HRSA Health Center Program requirements but do not receive Section 330 grant funding
- Must meet a stringent set of requirements, provide primary care services in underserved areas, offer a sliding fee scale and operate under a governing board that includes consumers
- Existing clinic(s) and/or practice(s) apply to become an FQHC Look-Alike and can maintain patient-provider continuity through an MSA
Maximize Medicaid managed care contracting strategy
FQHCs and similar organizations bring unique opportunities with relation to aligning incentives and maximizing quality and total cost of care revenue without negatively impacting PPS reconciliations.
It is important when contracting for value-based payment agreements with FQHCs that the various aspects such as capitation amount, quality bonus program and quality gating relationship to shared savings participation are taken into account.
Contact info@copehealhsolutions.com for assistance in achieving success on FQHCs.

