The New York State Medicaid Redesign team this week released a concept paper for a new 1115 Waiver, including a request for $17 billion over 5 years from the Centers for Medicare & Medicaid Services to build an enhanced health care delivery system as part of New York’s overall efforts to “reimagine, rebuild, and renew” in the wake of the COVID-19 crisis.
The state has outlined four goals to create a more equitable health care delivery system:
- Building a more resilient, flexible and integrated delivery system that reduces racial disparities, promotes health equity, and supports the delivery of social care
- Developing supportive housing and alternatives to institutions for the long-term care population
- Redesigning and strengthening health and behavioral health system capabilities to provide optimal response to future pandemics and natural disasters
- Creating statewide digital health and telehealth infrastructure
Major Takeaways
Here are five key points for New York payers and providers.
1. This is NOT your parents’ DSRIP-driven Medicaid Waiver
- Not a renewal or a “DSRIP 2.0.” Funding structures will look very different from the previous “retrospective reporting and performance bonus” format of DSRIP, but programs will leverage the lessons learned and positive wins from 10 years of DSRIP in previous waivers.
- Despite the different format, this waiver definitely looks to reform the delivery system, with a push towards value-based payments (VBP), integration of social determinants of health (SDOH) data and community-based organizations (CBO) along with traditional care delivery.
- Overall push to grow more community- based care outside the “four walls” of traditional health care delivery sites for the 7 million New York Medicaid members.
2. Continued focus on aligning managed care organizations and provider incentives by advancing capitation and global-budget, full-risk VBPs
- The New York State Department of Health will invest in advanced VBP models that fund coordination and delivery of social care through distribution to managed care organizations and qualifying VBP-contracted provider networks that integrate SDOH data and CBOs.
- Attribution methodologies will be expanded to include attribution to behavioral health providers, health homes, or care coordination organizations as appropriate rather than relying only on primary care attribution.
- VBP incentive pool will include a fee schedule to pay CBOs on a per-service basis or similar methodology as an additional cash flow mechanism to fund adequate investment in key initiatives rather than relying on shared savings at the end of a measurement period.
- Managed care organizations and provider networks are expected to expand beyond traditional health risk adjustments to include social risk adjustments in order to accommodate the impact of SDOH on the cost of care.

3. Two new organizational structures introduced – HEROs and SDHNs
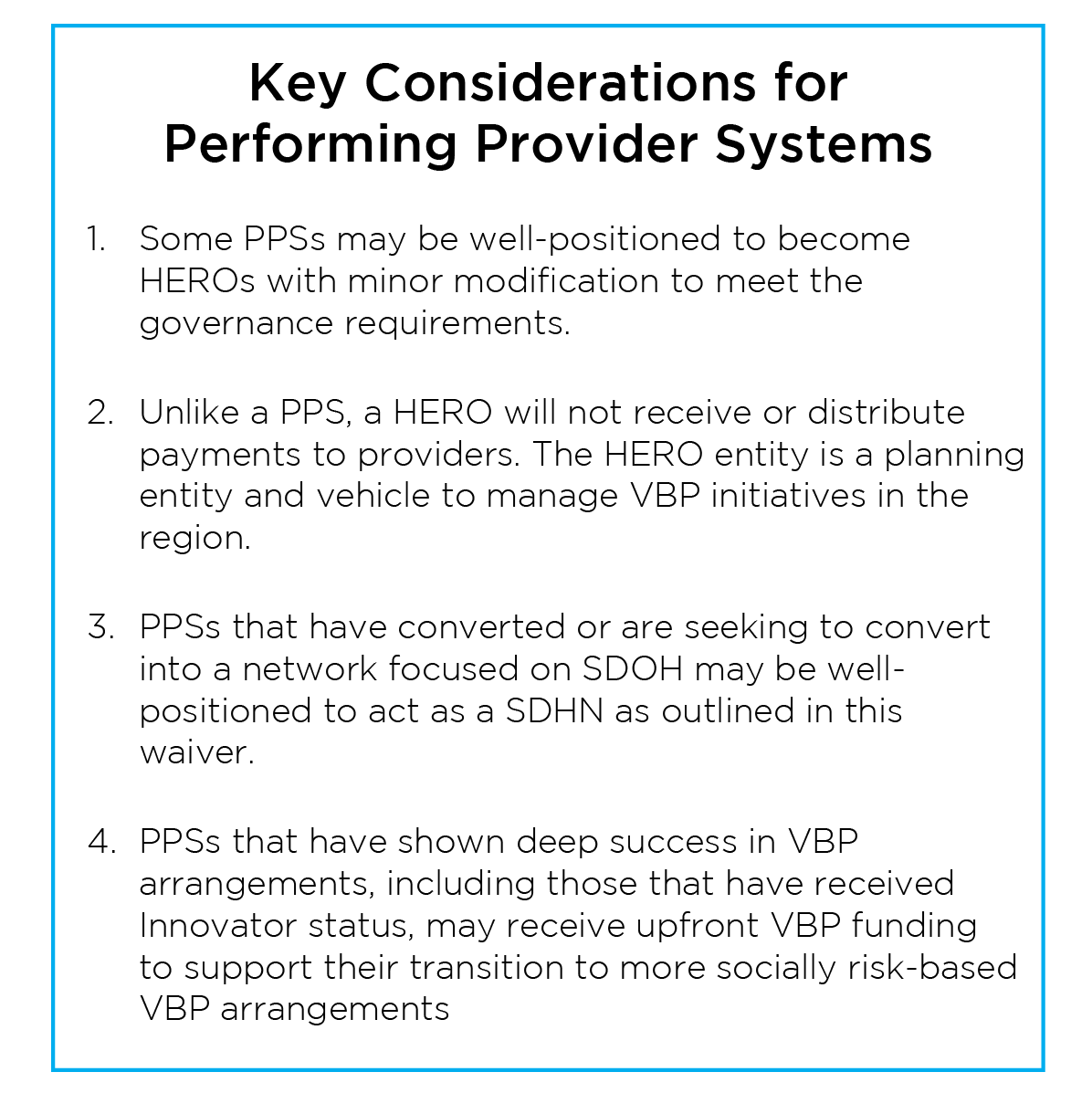
- Seven, possibly more, Health Equity Regional Organizations (HEROs), will be chosen to be regional mission-based coalitions of managed care organizations, hospitals and health systems, community-based providers, population health vehicles, independent physician associations (IPAs), behavioral health networks, long-term support and services, CBOs, qualified entities/regional health information organizations, consumers and others.
- HEROs will NOT be a funding intermediary but rather will receive “limited planning grants” and focus on ability to ingest data from government and proprietary sources for regional planning.
- Social Determinants of Health Networks (SDHN) will be another type of regional entity (overlapping with HERO regions) that organize CBOs into a contracting network which may look similar to an IPA.
- Eligibility has been expanded versus the 2019 New York State waiver proposal so that the lead entity coordinating a SDHN can be a single CBO, collaboration of multiple CBOs, or a Performing Provider System that seeks to convert into a CBO network management organization.
- SDHNs will receive funding for IT, business process implementation and other required infrastructure to support contracted CBOs while additional funds will flow directly to CBOs based on completion of project milestones and outcomes.
4. Additional funding streams focused on SDOH Needs and Health Equity
- Extends eligibility for Medicaid to incarcerated individuals up to 30 days prior to release in order to facilitate the transition into the community.
- Adds funding to support adequate housing access and provides alternatives to institutions for long-term care.
- Housing services and supports may be funded through VBP arrangements and through direct payments from HEROs.
5. Investment in workforce development and IT infrastructure
- Calls for substantial reinvestment in workforce investment organizations for a cohesive approach to regional workforce development focused on recruitment and retention initiatives and standardized training programs.
- Creates new career pathways and training foundations to expand community health workers, care navigators and peer support workers drawing from low-income and underserved communities.
- Launches an Equitable Virtual Care Access Fund to provide waiver funds to Medicaid providers that lack the financial capacity to invest in necessary IT Infrastructure and capabilities to support their attributed population.
What’s Next and What We Don’t Know Yet
The 1115 waiver demonstration proposal submitted this week is another step in the negotiation with CMS. The concept paper references the efforts to maintain budget neutrality but it is noticeably lacking details on funding streams to better understand the source of the $17 billion price tag and how New York State will keep its Medicaid budget neutral. We expect to be hearing more over in the coming months as this comes to fruition.
The COPE Health Solutions team of expert clinicians, finance leaders and operators includes some of the most experienced leaders in the country with relation to payer and provider risk arrangements, including all levels of capitation and over 20 years of supporting providers, payers and states to succeed in Medicaid Transformation Waiver programs in New York and across the nation.
Our team brings to bear unparalleled value-based payment and population health management expertise coupled with an adaptable set of solutions that range from advisory consulting to analytics with reporting support with our state-of-the-art Analytics for Risk Contracting (ARC) software. We also provide side-by-side implementation and joint operation of risk-bearing entities with aligned incentives.We have established and co-managed care management, utilization management and other managed service organization functions to allow clients to achieve financial and operational success in these models.
As the investments and new funds flows proposed in this waiver emphasize a migration to enhanced VBP models, our national expertise and data driven strategic support will help our clients plan for and navigate the proposed landscape.
For more information, please contact info@copehealthsolutions.com.

