Introduction
Hospital and health systems that strive toward value-based payment as their primary payor engagement strategy become more accountable for costs and health outcomes after a patient leaves an acute care facility. Medicare has already made this accountability a fact of life for all hospitals serving Medicare members through the value-based payment and re-admissions penalties assessed on those facilities without the right systems in place to ensure better performance. Post-acute care makes up a significant share of spending for health plans, costing, for some illnesses (e.g. congestive heart failure), nearly as much as a stay in the hospital.1 Addressing these costs has become an essential strategy for health systems looking to be successful, not only under bundled payment, ACO and capitated arrangements but even for Medicare fee for service due to the significant financial impact the VBP and re-admission penalties can represent.2
Recognizing this, systems across the country are developing high-quality networks of select skilled nursing facilities (SNFs) in order to improve quality outcomes and patient satisfaction, reduce total cost, streamline communication and ensure system-wide adoption of best practices.3
Background
In recent years, one of the nation’s largest public safety net hospital systems, serving over one million patients each year and operating several hospitals, outpatient clinics, SNFs, long term acute care facilities, and a variety of ancillary services across a large metropolitan area, has undertaken intensive efforts to reduce costs, increase performance, and improve care quality across the spectrum of care.
In 2016, post-acute leadership at the system began an initiative to develop a network of high-quality SNFs and other post-acute providers across their service area and to streamline the transition of patients from acute to post-acute care settings.
As one of the largest public hospital systems in the country, the development of a post-acute care network necessitated an especially robust procedure of assessment and system transformation. To achieve their goals, the enterprise embarked on a well-rounded approach, focusing on network selection, referral optimization, and IT infrastructure that resulted in targeted and sustainable SNF partnerships.
Our Approach
Post-acute leadership engaged in a three-pronged approach to building its network, using the following framework:
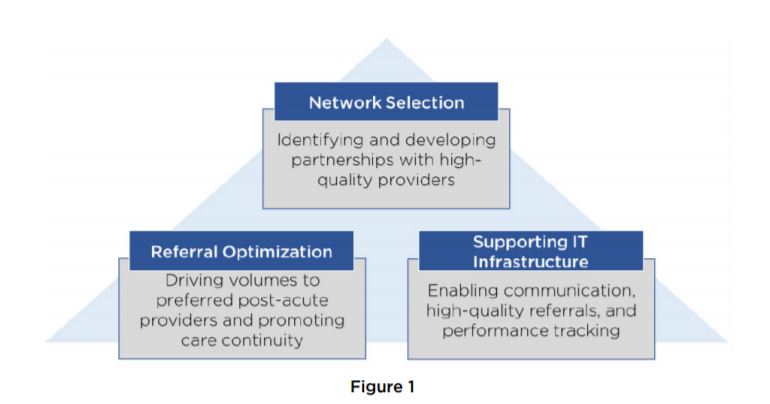
- Network Selection: The process of selecting and forming partnerships with SNFs was the focal point of the effort to build a successful network, ensuring that the right SNFs provide the right care in the right locations to meet the unique health and social needs of the population served.
- Referral Optimization: To maximize the utility of the network, post-acute leaders examined the existing hospital-to-SNF referral process, and designed protocols to enhance the choices offered to patients following discharge, minimize gaps in care quality and avoidable utilization, and increase use of preferred SNFs across the network.
- Enabling Technology Infrastructure: An optimal referral process must allow discharge planners to communicate with SNFs across care settings, identify high-quality SNFs within their network, and track SNF performance for quality and utilization. Robust technology platforms facilitate these processes, allowing for better informed and faster decision-making.
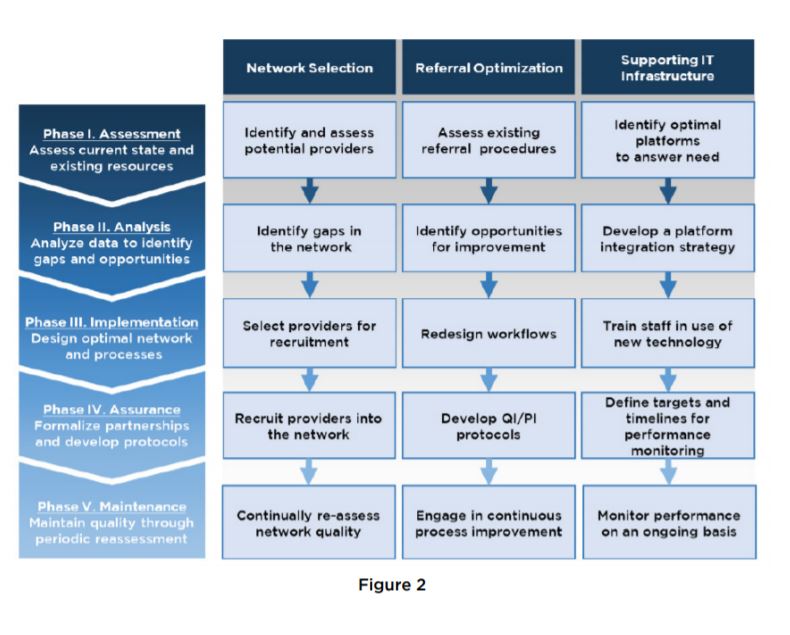
The post-acute team employed a phased process to simultaneously build each of these competencies. The grid below depicts the purpose of each phase within a particular area.

Key Activities and Results
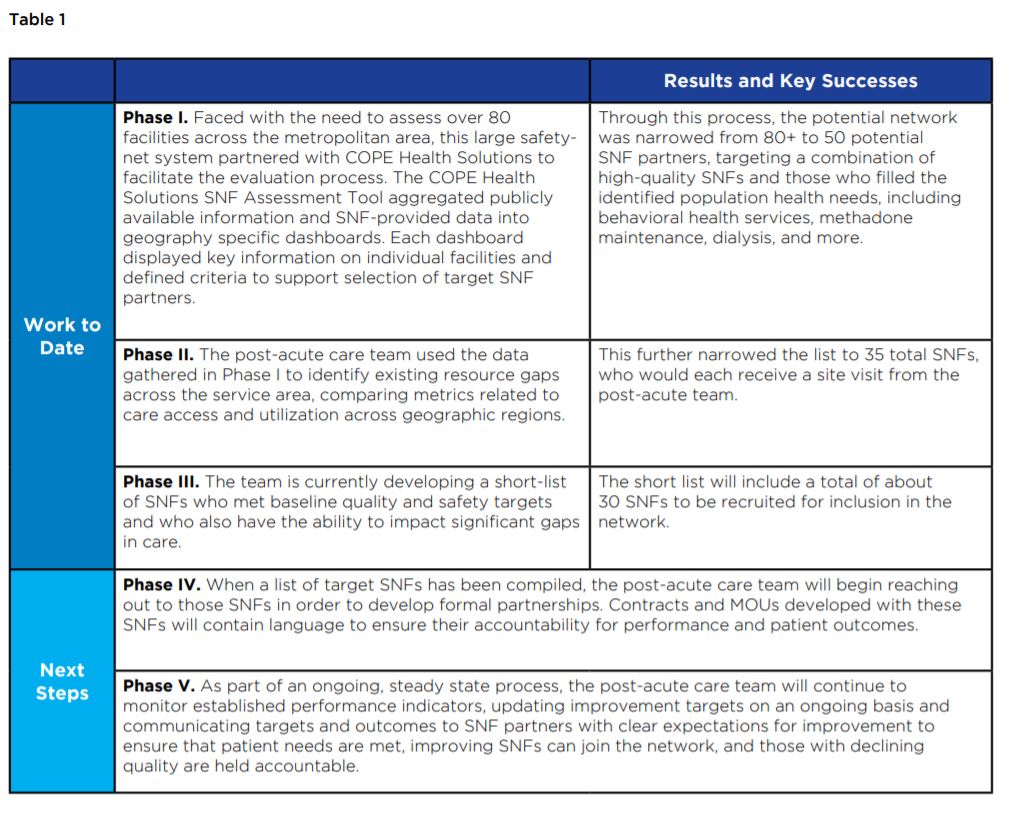
Network Selection
Identifying and targeting the right SNFs for the network necessitated a careful assessment of existing providers within the service area along quality, utilization, and financial metrics. The post-acute team worked with COPE Health Solutions to develop an evaluation framework and to gather and aggregate the data, ultimately producing a fully vetted list tailored to the needs of the patient population.

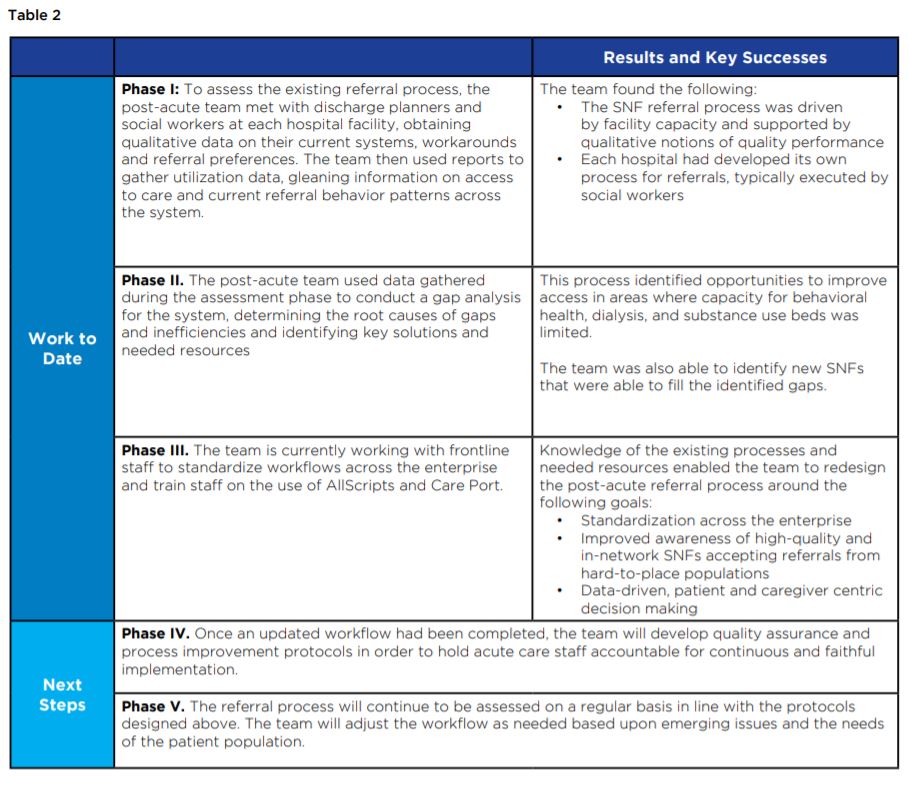
Referral Optimization
Post-acute leadership led a simultaneous effort to assess and optimize the existing acute- to post-acute referral pathways within the hospital system. The team met with frontline staff to understand existing protocols and develop more efficient strategies to quickly and easily identify SNFs that met the patients’ needs.

Supporting IT Infrastructure
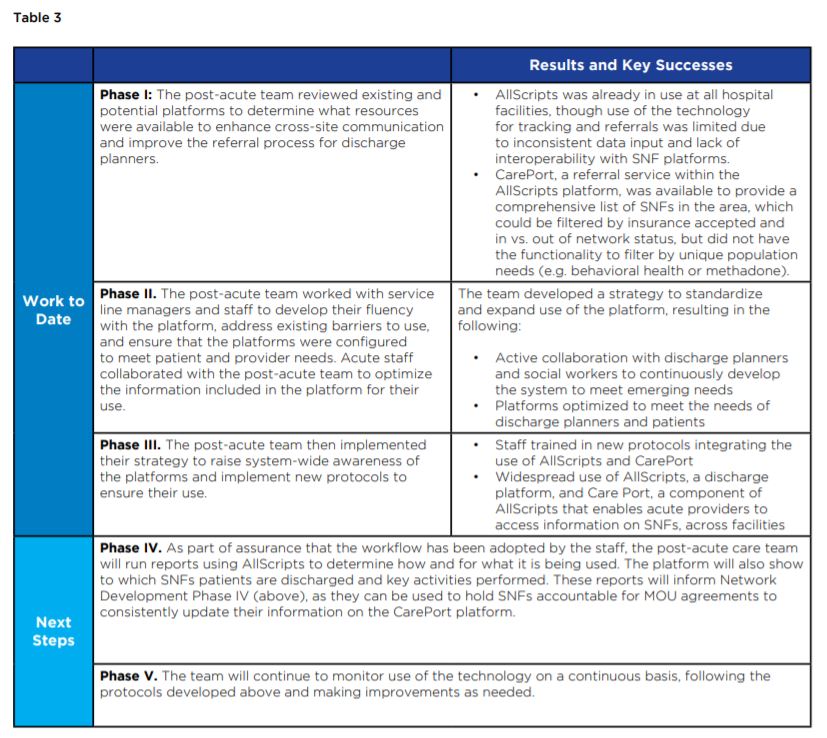
Recognizing the need for better access to information on post-acute providers and robust communication infrastructure, the post-acute team identified and began training staff in the use of existing technology platforms to meet their needs.

Conclusion
These efforts will produce a network of high-quality skilled nursing facilities that function within the system-wide provider network. Robust referral protocols and technological infrastructure will allow acute care staff to quickly and easily identify the SNFs that best meet the needs and desires of the patient, enabling seamless transitions from hospital to SNFs and lowering avoidable readmission rates. As the Post-Acute Division begins to gather data on financial, utilization, and quality performance across the enterprise, the team expects to see improvements in patient satisfaction and health outcomes with a simultaneous decrease in avoidable acute care utilization and overall cost of care for the SNF population.
Footnotes
1 Daly, R. (2016, April 14). Post-Acute Networks Are Biggest Hospital Challenge: Survey. Retrieved from https://www.hfma.org/Content.aspx?id=47684
2 Chandra, A., Dalton, M. A., & Holmes, J. (2013). Large Increases in Spending On Post-acute Care in Medicare Point to the Potential for Cost Savings in These Settings. Health Affairs, 32(5), 864-872. doi:10.1377/hlthaff.2012.1262 Hegwer, L. R. (2013, November 6). Bridging Acute and Post-Acute Care. Leadership. Retrieved from http://www.hfma.org/acutepostacute/
3 McClusky, M. E., FACHE (Presenter). (2016, May 17). Bundled Payment: The Role of Post-Acute Care in Emerging Health Care Networks. http://www.leadingageny.org/home/assets/File/Succeeding %20Under%20Bundled%20Payment_McClusky(1).pdf
4 Mechanic, R. (2014). Post-Acute Care — The Next Frontier for Controlling Medicare Spending. New England Journal of Medicine, 370(8), 692-694. doi:10.1056/nejmp1315607
5 Mor, V., Intrator, O., Feng, Z., & Grabowski, D. C. (2010). The Revolving Door Of Rehospitalization From Skilled Nursing Facilities. Health Affairs, 29(1), 57-64. doi:10.1377/hlthaff.2009.0629.
6 Samaris, D., & Allen, P. (2017, April 12). Developing a Post-Acute Care Network [PPT]. HFMA. www.hfma.org/DownloadAsset.aspx?id=536782.
7 Tyler, D. A., Gadbois, E. A., Mchugh, J. P., Shield, R. R., Winblad, U., & Mor, V. (2017). Patients Are Not Given Quality-Of-Care Data About Skilled Nursing Facilities When Discharged From Hospitals. Health Affairs, 36(8), 1385-1391. doi:10.1377/hlthaff.2017.0155
8 Griffin, K. M., & Gong, J. (2016, May 19). Hospitals Building a Successful Care Continuum | H&HN. https://www.hhnmag.com/articles/7194-hospitals-building-a-successful-care-continuum
