Background
The period following discharge as a patient transitions from hospital to home can be a vulnerable time for patients, especially those who are at high risk for hospital readmission. Preventable hospital readmissions often stem from a discontinuity in a patient’s care plan due to confusion surrounding discharge instructions, changes to medication regimen, or lack of understanding of important symptoms1. Not only can this result in care for effects for the patient, but this also can be financially costly for hospitals that accrue them2. Under the Hospital Readmissions Reduction Program, up to 3% of a hospital’s Medicare inpatient payments are at risk if patients return to the hospital within 30 days of discharge for specific medical conditions, such as acute myocardial infarctions, heart failure, pneumonia, and chronic obstructive pulmonary disease3.
Increased communication with patients post-discharge can promote effective transitions of care from hospital to home4. An effective mode of increasing communication is through post-discharge phone calls, which, when conducted within 48 to 72 hours after discharge, have successfully reduced hospital readmission rates and boosted patient satisfaction5,6,7.
The Problem
A common challenge many hospitals face with post-discharge phone calls is finding the staff and time to effectively manage the calls, which can accumulate rapidly. These were the barriers that St. Mary Medical Center (SMMC) in Long Beach, CA faced when addressing post-discharge phone calls on its medical surgical and telemetry floors. The task of handling the load of post-discharge calls proved to be difficult and un-sustainable for front-line staff to tackle in addition to the direct patient care duties performed.
The Solution: Clinical Care Extenders Lend a Hand
Fortunately, an ideal solution was already in place at SMMC through its partnership with COPE Health Solutions. SMMC originally partnered with COPE Health Solutions in 2004 to implement the Clinical Care Extender (CCE) program. This program aims to bring aspiring health care professionals into the hospital and administrative setting to receive hands-on, experiential education. More than 300 active CCEs rotate in 17 hospital departments at SMMC to provide support to staff and patients. Engaging CCEs to conduct calls not only provided the resources to tackle the large call load, but also provided front-line staff the bandwidth to care for patients actively on the unit, thus enhancing the in-house patient experience. This activity also allowed CCEs to expand their experience and learning around patient care post-discharge. Through this collaboration, SMMC sought to achieve an increase in the number of discharge phone call attempts, as well as an increase in the number of patient interviews.
COPE Health Solutions recruited and trained a group of three to five CCEs per unit to participate in the project on a quarterly basis. The training for post-discharge phone calls layered on top of the initial 30-hour training all CCEs are required to attend prior to beginning the program. With an introduction to patient care and patient interaction, CCEs engaged in this project dove deeper in a specialized training on service excellence, telephone skills, and orientation to a pre-approved script. CCEs were also trained on how to escalate calls to front-line nursing staff when they required clinical intervention. Three attempts were made to contact each patient, and calls were marked ‘complete’ if the patient was interviewed and all questions were answered, or if a third unsuccessful attempt was made.
Barriers Uncovered
In addition to performing the calls, CCEs also collected data that was passed along to leadership to improve hospital operations. This data was reviewed by COPE Health Solutions with the nursing unit directors during bi-weekly meetings to obtain feedback and address any concerns requiring attention.
Based on the data collected, COPE Health Solutions identified five key barriers to successfully completing a post-discharge phone call at SMMC and proposed the following solutions:
- Inaccurate patient phone number. Work with admitting and front-line staff to ensure accurate information is captured upon admission and then confirmed upon discharge.
- Low interview rate on the third attempt. Remove the third attempt to ensure each patient can be reached in the 48-72 hour window.
- Difficult for patients to call facility back. Designate personnel for the patients to contact.
- Paper forms bottleneck the process. Implement an electronic post-discharge call tracking system once SMMC is fully transitioned to electronic health records.
- Quantity of time and effort influencing attempt volume. Strategize plan around staff and CCE engagement to continue to increase volume of phone calls.
Results and Discussion
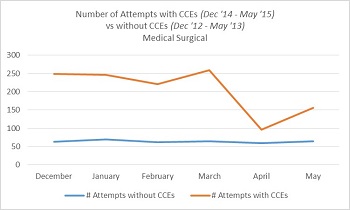
During the pilot phase from December 2014 to May 2015, the average number of post-discharge phone call attempts on the Medical Surgical unit increased by 219% when compared to the same time period two years prior. The average number of patient interviews also increased by 55%. Similarly, the average number of post-discharge phone call attempts on the Telemetry unit increased by 43% when compared the same time period the previous year. The average number of interviews on Telemetry was comparable to that of the previous year, most likely attributed to processes that the Telemetry unit had already put in place prior to the start of the pilot. The number of attempts made were directly influenced by the number of CCEs involved in the project, attributing to the fluctuation in attempt numbers.
Figure 1. Number of Attempts with CCEs (Dec’14-May’15) vs without CCEs (Dec ’12-May ’13) on Medical Surgical
 Figure 2. Number of Attempts with CCEs (Dec’14-May’15) vs without CCEs (Dec ’13-May ’14) on Telemetry
Figure 2. Number of Attempts with CCEs (Dec’14-May’15) vs without CCEs (Dec ’13-May ’14) on Telemetry
Conclusion
Engaging CCEs in making post-discharge phone calls proved to be an ideal solution to increase the number of phone call attempts and interviews, enable nursing staff to focus their time where it is needed most—delivering high quality patient care.
For more information, please contact:
Roya Mirilavassani
Manager
rmirilavassani@copehealthsolutions.org
References:
- Kripalani, Sunil, Frank Lefevre, Christopher O. Phillips, Mark V. Williams, Preetha Basaviah, and David W. Baker. “Deficits in Communication and Information Transfer Between Hospital-Based and Primary Care Physicians.” Jama8 (2007): 831. Web.
- Anderson, Gerard F., and Earl P. Steinberg. “Hospital Readmissions in the Medicare Population.” New England Journal of Medicine21 (1984): 1349-353. Web.
- Better Care, Smarter Spending, Healthier People: Improving Our Health Care Delivery System.” Centers for Medicare & Medicaid Services. N.p., 26 Jan. 2015. Web. 17 July 2015.
- Readmissions Reduction Program.” Centers for Medicare & Medicaid Services. N.p., 4 Aug. 2014. Web. 17 July 2015.
- Kripalani, Sunil, Amy T. Jackson, Jeffrey L. Schnipper, and Eric A. Coleman. “Promoting Effective Transitions of Care at Hospital Discharge: A Review of Key Issues for Hospitalists.” Journal of Hospital Medicine. 2.5 (2007): 314-23. Web.
- Checklist for Post-Discharge Follow-up Phone Calls: Project RED (Re-Engineered Discharge) Training Program.” Agency for Healthcare Research and Quality. N.p., Aug. 2011. Web.
- Harrison, Patricia L., Pamela A. Hara, James E. Pope, Michelle C. Young, and Elizabeth Y. Rula. “The Impact of Postdischarge Telephonic Follow-Up on Hospital Readmissions.” Population Health Management1 (2011): 27-32. Web.
- Braun, Eyal, Amjad Baidusi, Gideon Alroy, and Zaher S. Azzam. “Telephone Follow-up Improves Patients Satisfaction following Hospital Discharge.” European Journal of Internal Medicine2 (2009): 221-25. Web.